Answer to Question 1
D
The skill of applying a restraint can be delegated to trained nursing assistive personnel. However, the nurse is responsible for assessing a patient's behavior, determining the need for restraint, the type of restraint to use, and performing patient assessments while restraints are in place. Patients, who are confused, disoriented, or who repeatedly fall or try to remove medical devices (e.g., IV lines or dressings) may require the temporary use of restraints to keep them safe. Restraints are not a solution to a patient problem but rather a temporary means to maintain patient safety. All alternatives must be used before placing patients in restraints. Performing an assessment, obtaining orders from the physician and including the family in the discussion of why restraints are necessary are all jobs that cannot be delegated to a nursing assistive personnel (NAP); and must be performed by the nurse.
Answer to Question 2
B
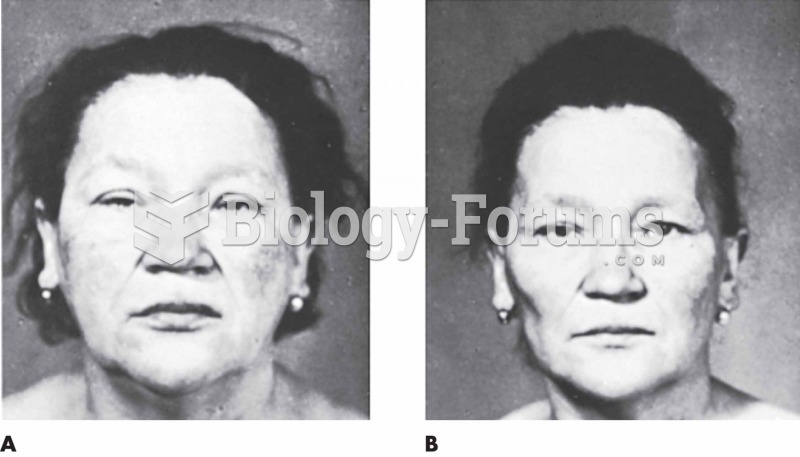
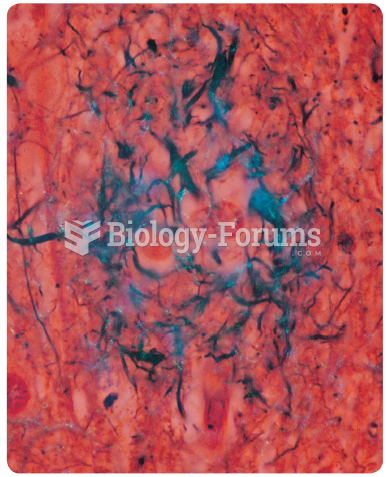
Shear is the force exerted against the skin while the skin remains stationary and the bony structures move. For example, when the head of the bed is elevated, gravity causes the bony skeleton to pull toward the foot of the bed, while the skin remains against the sheets. Friction is surface damage caused by the skin rubbing against another surface that often results in an abrasion. Friction would result if the patient is dragged across the sheets. Skin moisture increases the risk for ulcer formation as moisture softens the skin and reduces its resistance to other physical factors such as pressure or shear. Moisture comes from many sources such as wound drainage, perspiration, and/or fecal and urinary incontinence. With continuous pressure over the area, deep tissue destruction continues, which often results in larger pockets of necrotic tissue beneath the opening of the main wound that resemble a tunnel; this is referred to as tunneling.