Answer to Question 1
What do you do for someone who has delusions, hears his dead uncle's voice, or can't communicate complete thoughts? The search for help has taken many paths, sometimes down some disturbing roads; for example, in the 1500s primitive surgery was conducted to remove the stone of madness, which was thought to cause disturbed behavior. As barbaric as this practice may seem today, it is not different from the prefrontal lobotomies performed on people with schizophrenia as late as the 1950s. This procedure severed the frontal lobes from the lower portion of the brain, which sometimes calmed the patient but also caused cognitive and emotional deficits.
Researchers have assumed for more than 100 years that schizophrenia requires some form of biological intervention. Kraepelin, who so eloquently described dementia praecox in the late 19th century, saw the disorder as a brain disease. Lacking a biological treatment, he routinely recommended that the physician use good patience, kindly disposition, and self-control to calm excited patients (Nagel, 1991).
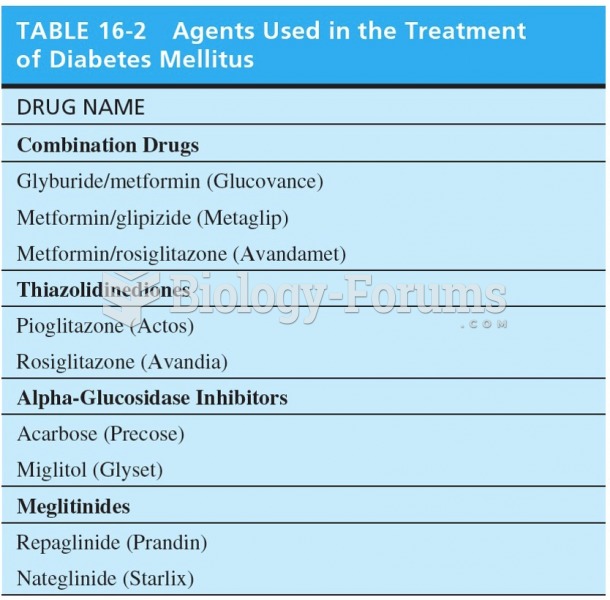
During the 1930s, several novel biological treatments were tried. One approach was to inject massive doses of insulinthe drug that given in smaller doses is used to treat diabetesto induce comas in people suffering from schizophrenia. Insulin coma therapy was thought for a time to be helpful, but closer examination showed it carried great risk of serious illness and death. During this time, psychosurgery, including prefrontal lobotomies, was introduced, and in the late 1930s, electroconvulsive therapy (ECT) was advanced as a treatment for schizophrenia. As with earlier drastic treatments, initial enthusiasm for ECT faded because it was found not to be beneficial for most people with schizophreniaalthou gh it is still used with a limited number of people today, sometimes in combination with antipsychotic medications.
A breakthrough in the treatment of schizophrenia came during the 1950s with the introduction of several drugs that relieved symptoms in many people. Called neuroleptics (meaning taking hold of the nerves), these medications provided the first real hope that help was available for people with schizophrenia. When they are effective, neuroleptics help people think more clearly and reduce hallucinations and delusions. They work by affecting the positive symptoms (delusions, hallucinations, and agitation) and to a lesser extent the negative and disorganized ones, such as social deficits. In general, each drug is effective with some people and not with others. Clinicians and patients often must go through a trial-and-error process to find the medication that works best, and some individuals do not benefit significantly from any of them. The earliest neuroleptic drugs, called conventional or first-generation antipsychotics (such as Haldol and Thorazine), are effective for approximately 60 percent of people who try them. However, many people are not helped by antipsychotics or experience unpleasant side effects. Fortunately, some people respond well to newer medicationssometime s called atypical or second-generation antipsychotics; the most common are risperidone and olanzapine. These newer drugs hold promise for helping patients who were previously unresponsive to medications.
Answer to Question 2
Historically, a number of psychosocial treatments have been tried for schizophrenia, reflecting the belief that the disorder results from problems in adapting to the world because of early experiences. Many therapists have thought that individuals who could achieve insight into the presumed role of their personal histories could be safely led to deal with their current situations. Although clinicians who take a traditional psychodynamic or psychoanalytic approach to therapy continue to use this type of treatment, research suggests that their efforts at best may not be beneficial and at worst may be harmful.
Today, few believe that psychological factors cause people to have schizophrenia or that traditional psychotherapeutic approaches will cure them. Nevertheless, you will see that psychological methods have an important role. Despite the great promise of drug treatment, the problems with ineffectiveness, inconsistent use, and relapse suggest that by themselves, drugs may not be effective with many people. As with a number of the disorders discussed in this text, recent work in the area of psychosocial intervention has suggested the value of an approach that uses both kinds of treatment.
An environment was designed for inpatients that encouraged appropriate socialization, participation in group sessions, and self-care such as bed making while discouraging violent outbursts. An elaborate token economy was set up, in which residents could earn access to meals and small luxuries by behaving appropriately. A patient could, for example, buy cigarettes with the tokens he earned for keeping his room neat. On the other hand, a patient would be fined (lose tokens) for being disruptive or otherwise acting inappropriately. This incentive system was combined with a full schedule of daily activities. Patients who went through their program did better than others on social, self-care, and vocational skills, and more of them could be discharged from the hospital. Problems with social skills can be the most visible impairment displayed by people with schizophrenia and can prevent them from getting and keeping jobs and making friends. Clinicians attempt to re-teach social skills such as basic conversation, assertiveness, and relationship building to people with schizophrenia.