Answer to Question 1
No. His systolic blood pressure is too high (152 mm Hg), he is tachycardic (124 beats/min) and
tachypneic (42 breaths/min), and his temperature is elevated at 100.4 F. B.T. is anxious and
experiencing shortness of breath. His respiratory muscles are working hard to breathe, thereby
increasing his metabolic rate, temperature, and stress.
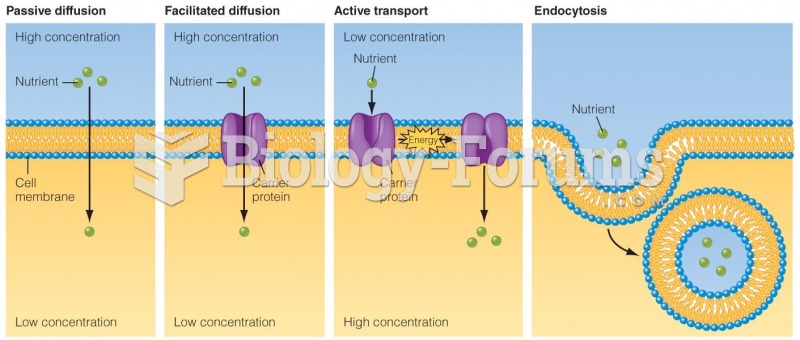
Bronchoconstriction has caused an increase in airway resistance and a decrease in tidal volume. The goal of therapy is to compensate by increasing the concentration of inspired O2.
General: Note his position: Is he upright or forward leaning? Does he appear restless or exhausted?
What is his mental status? Is he confused or agitated?
Respiratory: Auscultate lung sounds, listening for wheezing, crackles, diminished or absent breath
sounds, and rhonchi. Percuss for any areas of hyperresonance. Observe for the presence of any
sputum, increased work of breathing with use of accessory muscles or retractions, or prolonged
expiration.
Integumentary: Note skin color and the presence of any diaphoresis.
Cardiovascular: Assess for the presence of pulsus paradoxus and jugular venous distention. Are there premature ventricular contractions or other dysrhythmias on the electrocardiogram (ECG)?
B.T.'s pH indicates that he is acidotic. His Paco2 level is high, which indicates that he is retaining
carbon dioxide, consistent with poor respiratory function. This means B.T. has respiratory acidosis.
His bicarbonate level is within normal limits. B.T. lives at high altitude. Although his Pao2 will be
decreased at this altitude, his Spo2 should be above 90; the 88 Spo2 and the Pao2 of 55 indicate that hypoxemia related to the asthma attack is at a level that could indicate impending respiratory failure.
Albuterol (e.g., Ventolin, Proventil) is a fast-acting beta2 agonist that acts to relax and open airways
and increase ciliary movement to help clear secretions. It may cause shakiness, nervousness,
tachycardia, and/or increased BP, so B.T. should be closely monitored. Ipratropium is an
anticholinergic that causes bronchodilation and inhibits secretions without causing systemic
anticholinergic effects. The combination is more effective than either drug alone.
Metaproterenol sulfate is a short-acting beta2 receptor adrenergic bronchodilator. It is used to
reverse airway constriction caused by acute and chronic bronchial asthma. Because it has a rapid
onset of action (a few minutes), it is used to treat acute bronchospasm. During acute exacerbations,
it can be used every 3 to 4 hours. Fluticasone (Flovent), an inhaled corticosteroid, is used to control
the inflammatory response that is believed to be a cause of asthma. It is often used concurrently
with bronchodilators, primarily beta-adrenergic agonists. Flovent is typically taken twice daily. The
use of this combination should reduce swelling, mucus production, and spasm in and of the airways,
resulting in the easing of airway constriction.
Answer to Question 2
S.R. needs to have a working knowledge of the CPAP system.
How to apply the mask and connect it to the machine
How to manage the fit of CPAP mask or nasal device to reduce irritation and discomfort
Ways to decrease anxiety associated with wearing the CPAP system
How to perform daily equipment maintenance and clean the system
What to do in case of respiratory distress or other complications
Ask the durable medical equipment (DME) company to check for proper fitting of the mask and
tubing and whether adding humidification to his O2 is possible.
Get saline nasal spray at any drugstore or make your own. Use two sprays in each nostril up to
every 2 hours as needed. A recipe for ocean saline spray: Boil water 20 minutes and let cool. Then
to 1 quart of water, add 1 teaspoon of salt, plus a pinch of baking soda. Store at room temperature
in a covered container for up to 72 hours, and then discard.
Describe how to pad and protect the skin behind his ears.
Have him gently cleanse the nares every 8 hours with a cotton-tipped applicator moistened with
saline.
First, state the date and time of the phone call and who was on the phone providing information.
Then describe the subjective information provided by S.R., providing enough detail to support the
plan of action and justify that his problem can be managed without an in-person visit. In this case,
you would document his complaints of dry nasal membranes, nosebleeds, and sores behind the ears,
noting details of your assessment, such as when symptoms started and symptom severity. You would
then detail the plan of action, describing the care instructions given him, concluding with when and
how to seek additional care.