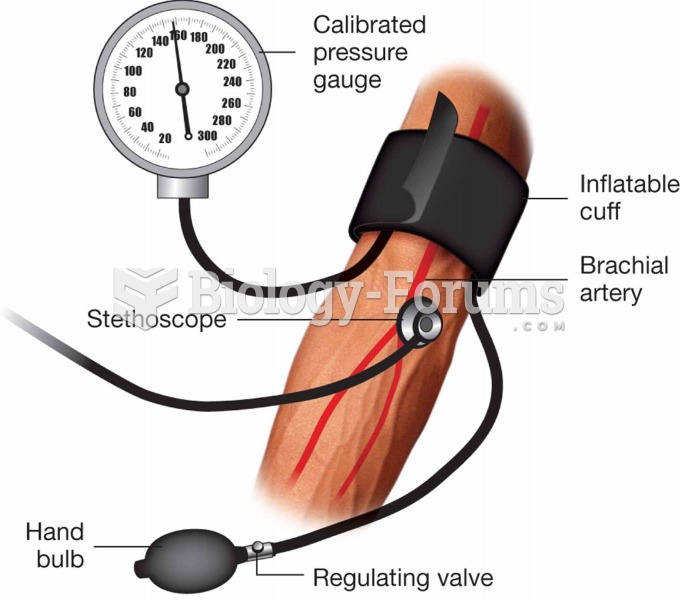
During the episode of chest pain, R.K.'s vital signs were as follows: pulse 110 beats/min; blood pressure 140/92 mm Hg, respirations 20 breaths/min.
The rhythm strip shows sinus tachycardia, and she was very
anxious. Her chest discomfort subsided in 3 minutes after one nitroglycerin dose, and she is resting quietly
with O2 per nasal cannula at 2 L/min. R.K.'s physician is making rounds.
Using SBAR (Situation, Background, Assessment, Recommendation), how would you
communicate this episode to R.K.'s physician?
Question 2
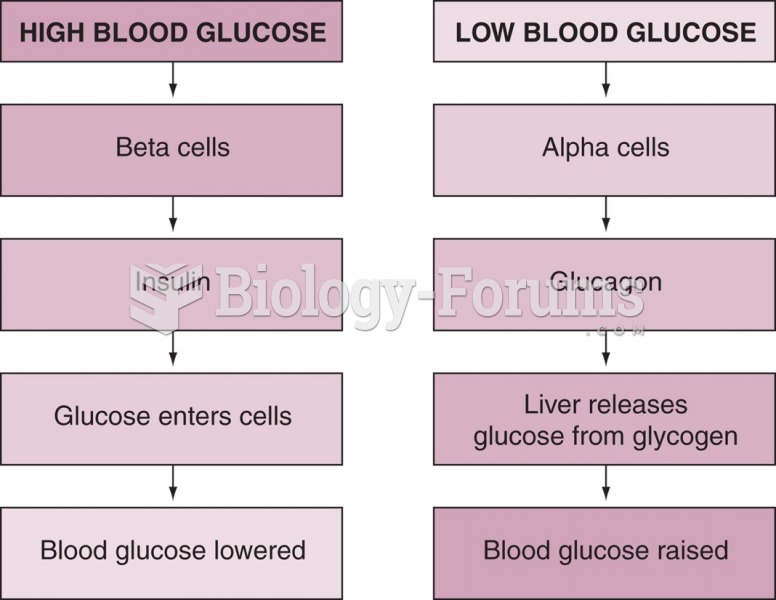
After some rest, R.K.'s chest pain has subsided, and she tells you she feels much better now. You review her laboratory results.
Laboratory Results
12-lead ECG: Light left-axis deviation, normal sinus rhythm with no ventricular ectopy
Serial CPK tests are 30 units/L at admission, 32 units/L 4 hours after admission
Cardiac troponin T is less than 0.01 ng/mL (at admission) and same result 4 hours after admission
Cardiac troponin T is less than 0.03 ng/mL (at admission) and same result 4 hours after admission
D-dimer test result less than 250 ng/mL
On the basis of the information presented so far, do you believe she had an MI? What is your
rationale?
Do you think she may have a pulmonary embolus?
While you care for R.K., you carefully observe her. Identify two possible complications of
coronary artery disease (CAD) and the signs and symptoms associated with each.
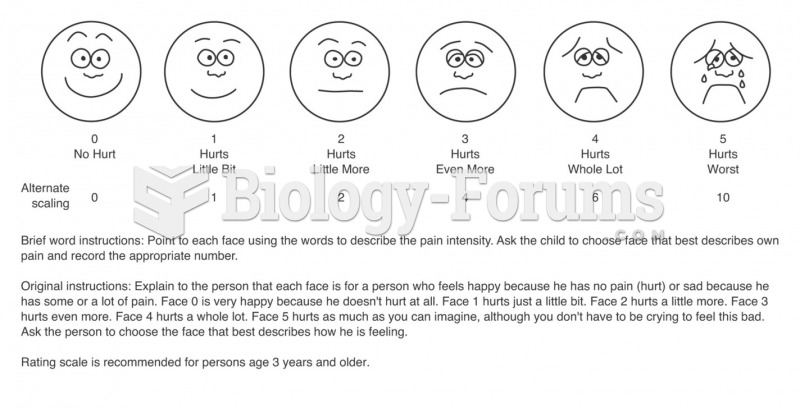
R.K. rings her call bell. When you arrive, she has her hand placed over her heart and tells
you she is having that heavy feeling again. She is not diaphoretic or nauseated, but states
she is short of breath. What else do you assess, and what can you do to make her more
comfortable?