Answer to Question 1
A
The age-related change that would affect airway clearance is decreased defense mechanisms, whereby the patient will have difficulty excreting anesthesia gas. The nurse needs to monitor the patient's oxygen status carefully to make sure the patient does not retain too much of the drug. Heart muscle thickening and mental status do not affect oxygenation in patients undergoing anesthesia. Lung capacity is not related to anesthesia induction.
Answer to Question 2
C
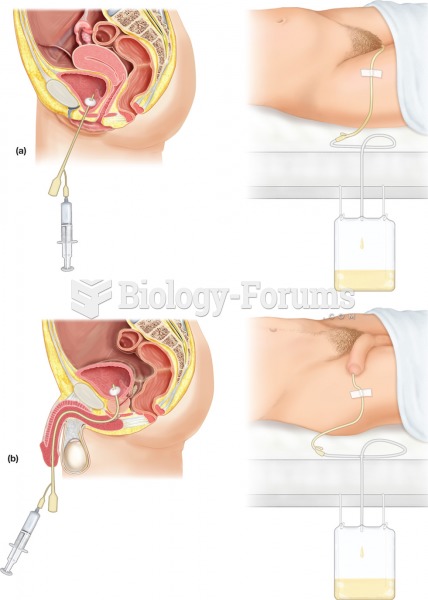
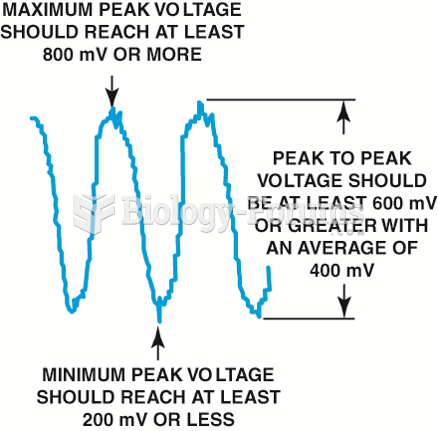
Monitoring vital signs every 15 minutes is the highest priority. When clients are receiving epidural analgesia, monitoring occurs as often as every 15 minutes, including assessment of respiratory rate, respiratory effort, and skin colour. Once the client is stabilized, monitoring can move to every hour (the nurse should the employer policy). Complications of epidural opioid use include nausea and vomiting, urinary retention, constipation, respiratory depression, and pruritus. A common complication of epidural anaesthesia is hypotension. Assessing vital signs is the priority nursing intervention.
Using aseptic technique is also important, but not the highest priority. Because of the catheter location, strict surgical asepsis is needed to prevent a serious and potentially fatal infection.
To reduce the risk of accidental epidural injection of drugs intended for IV use, the catheter should be clearly labelled epidural catheter. This should be done when catheter is inserted.
The nurse explains insertion and what is expected to the client, and prepares the client for dis-comfort he or she may encounter. However, this is not the priority nursing intervention.