This topic contains a solution. Click here to go to the answer
|
|
|
Did you know?
Critical care patients are twice as likely to receive the wrong medication. Of these errors, 20% are life-threatening, and 42% require additional life-sustaining treatments.
Did you know?
If all the neurons in the human body were lined up, they would stretch more than 600 miles.
Did you know?
According to the National Institute of Environmental Health Sciences, lung disease is the third leading killer in the United States, responsible for one in seven deaths. It is the leading cause of death among infants under the age of one year.
Did you know?
Multiple sclerosis is a condition wherein the body's nervous system is weakened by an autoimmune reaction that attacks the myelin sheaths of neurons.
Did you know?
The ratio of hydrogen atoms to oxygen in water (H2O) is 2:1.
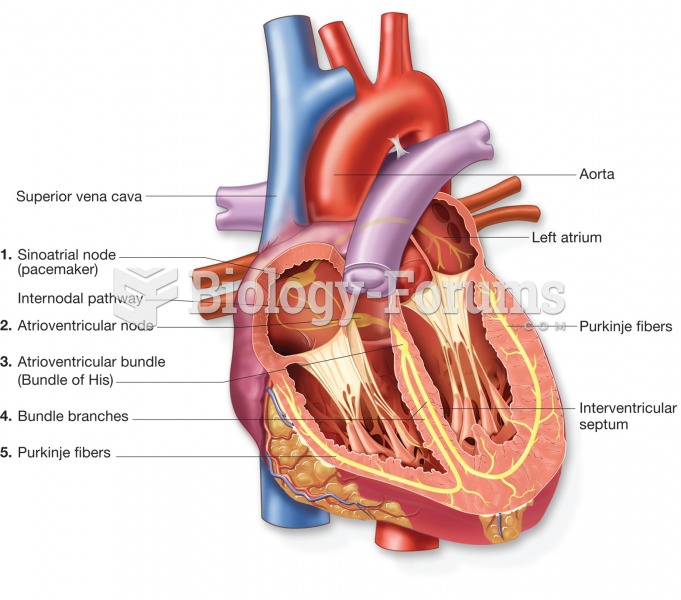 The conduction system of the heart; traces the path of the electrical impulse that stimulates the he
The conduction system of the heart; traces the path of the electrical impulse that stimulates the he
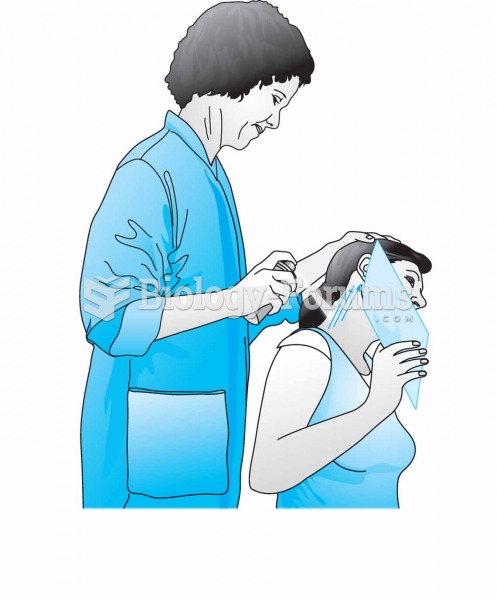 Vapocoolant spray application while passively stretching the paracervical muscles. Take care to prot
Vapocoolant spray application while passively stretching the paracervical muscles. Take care to prot