Answer to Question 1
Answer:
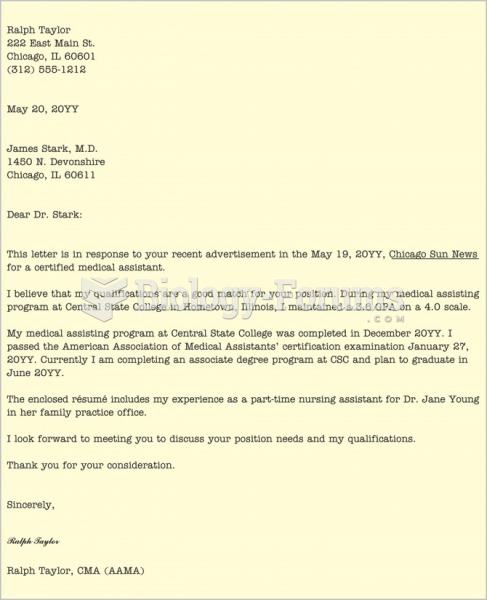
An anesthesiologist may be classified as either a hospital staff anesthesiologist (employed by the hospital) or an independent anesthesiologist (self-employed or not employed by the hospital). Charges made by a hospital for the services of a staff anesthesiologist are usually covered as a hospital ancillary expense.
Charges by an outside anesthesiologist vary according to plan provision, but are usually covered under either a separate Basic anesthesia benefit or under a Major Medical benefit.
Anesthesia may be administered by any of the following individuals:
Medical doctor (MD)
Anesthesiologist (Anes.)
Certified Registered Nurse Anesthetist (CRNA)
Anesthetic Assistant (AA)
Answer to Question 2
Answer:
Same Time, Different Operative Field
When more than one surgery is performed during the same operative session but through a different orifice (opening) or incision or in a different operative field, 100 of the UCR is allowable for the major procedure, and 50 of the UCR (or actual charge, whichever is less) is allowed for the second procedure. 25 of UCR (or actual charge, whichever is less) is allowed for each additional procedure. Some insurance carriers, however, do not apply the 25 rule, allowing 100 for the primary procedure and 50 thereafter. Bilateral procedures have the same rules as multiple procedures performed through different incisions. Multiply the UCR allowance for the single procedure by 150 or 1.5. If there is an established bilateral CPT code, that code would be allowable at 100 only because the units have already been assigned at 150 of the unit value for the single procedure. There are two ways to identify a bilateral procedure. The provider will list the CPT and use modifier -50 to denote a bilateral procedure. Sometimes the provider will identify LT (left) or RT (right) next to each procedure. When in doubt, obtain an operative report.
Same Time, Same Operative Field
When multiple procedures are performed during the same operative session through the same incision, orifice, or operative field, the additional procedures are usually considered to be incidental.