Answer to Question 1ANS: D
Do not include any reference to an incident in the medical record; therefore, the nurse manager must follow up. A notation about an incident report in a patient's medical record makes it easier for a lawyer to argue that the reference makes the incident report part of the medical record and therefore subject to attorney review. When an incident occurs, document an objective description of what happened, what you observed, and the follow-up actions taken, including notification of the patient's health care provider in the patient's medical record. Remember to evaluate and document the patient's response to the incident.
Answer to Question 2ANS: D
You need to ensure the information within a recorded entry or a report is complete, containing appropriate and essential information (pain of

. Document subjective and objective assessment. While pupils equal and reactive to light is data, it does not relate to the chest pain; this information would be critical for a head injury. Derogatory or inappropriate comments about the patient or family (pain) is not appropriate. This kind of language can be used as evidence for nonprofessional behavior or poor quality of care. Avoid using generalized, empty phrases like poor results. Use complete, concise descriptions.
Answer to Question 3ANS: C
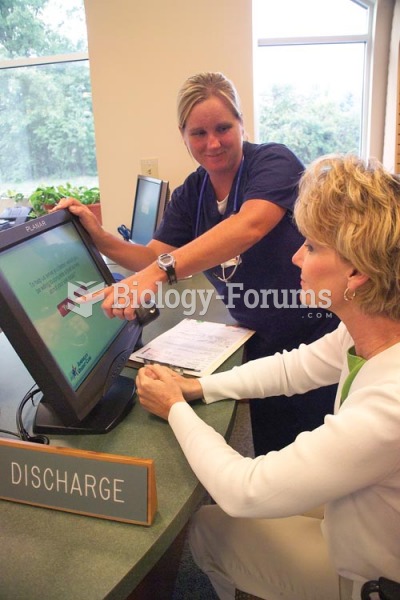
One design model for Nursing Clinical Information Systems (NCIS) is the protocol or critical pathway design. This design facilitates interdisciplinary management of information because all health care providers use evidence-based protocols or critical pathways to document the care they provide. The knowledge base within a CDSS contains rules and logic statements that link information required for clinical decisions in order to generate tailored recommendations for individual patients, which are presented to nurses as alerts, warnings, or other information for consideration. The nursing process design is the most traditional design for an NCIS. This design organizes documentation within well-established formats such as admission and postoperative assessments, problem lists, care plans, discharge planning instructions, and intervention lists or notes. Computerized provider order entry (CPOE) systems allow health care providers to directly enter orders for patient care into the hospital's information system.