Answer to Question 1
ANS: 1
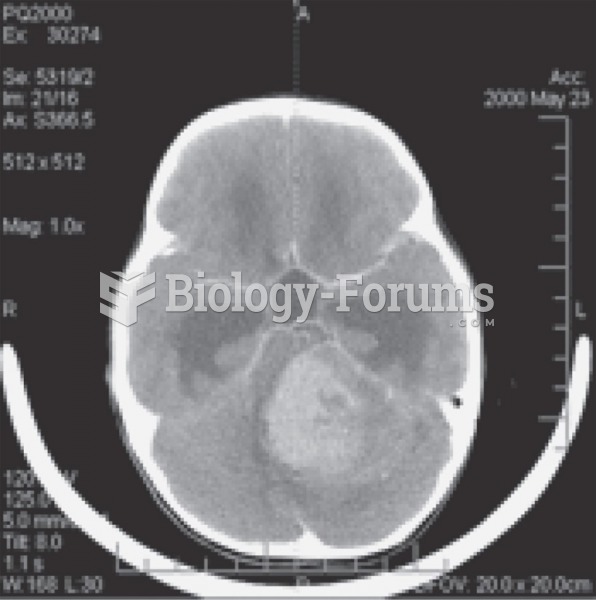
The most common language disorder following a stroke is aphasia. As a result of a disruption in blood flow to the brain, the speech center becomes damaged, altering a person's ability to either use or understand spoken words. Depending on the type of aphasia, the inability to communicate is often frustrating and frightening. Initially you need to establish very basic communication and recognize that aphasia does not indicate intellectual impairment or degeneration of personality. Explain situations and treatments that are pertinent to the client because he or she is able to un-derstand the speaker's words. Because a stroke often causes partial or complete paralysis of one side of the client's body, an aphasic client will need special assistive devices. There are commu-nication boards that have been developed for several levels of disability. Sensitive pressure switches, activated by the touch of an ear, nose, or chin, control electronic communication boards. Clients who have had a stroke usually acquire referrals to speech therapists to develop appropriate rehabilitation plans.
Answer to Question 2
ANS: 2
In the case of sensory alterations you need to integrate knowledge of the pathophysiology of sensory deficits, factors that affect sensory function, and therapeutic communication principles. A person's occupation places him or her at risk for hearing, visual, and peripheral nerve altera-tions. Individuals who have occupations involving exposure to high noise levels (e.g., factory or airport workers) are at risk for noise-induced hearing loss and need to be screened for hearing impairments. Hazardous noise is common in work settings as well as recreational activities. Be careful to not automatically assume that a client's sensory problem is related to advancing age. For example, adult sensorineural hearing loss is often due to exposure to excess and prolonged noise or metabolic, vascular, and other systemic alterations. Collect a history that also assesses the client's current sensory status and the degree to which a sensory deficit affects the client's life-style, psychosocial adjustment, developmental status, self-care ability, health promotion habits, and safety.