Answer to Question 1
ANS: 3
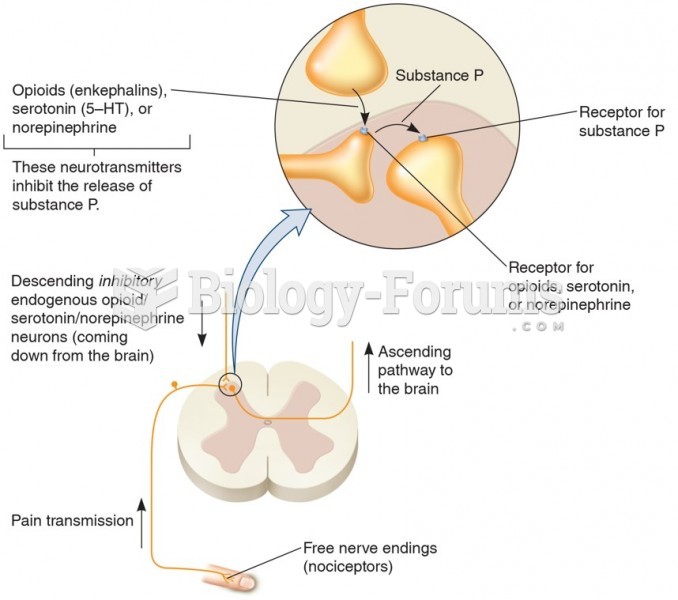
The possible unknown cause of noncancer pain, combined with the unrelenting pain and uncer-tainty of its duration, frustrates the client, frequently leading to psychological depression and perhaps suicide. There is no evidence to demonstrate a relationship between chronic pain and criminal activity. Health care workers are usually less willing to treat chronic noncancer pain with opioids, although a recent policy statement supports the use of opioids for noncancer pain. In ad-dition, the American Society of Anesthesiologists developed the Practice Guidelines for Chronic Pain Management, which includes the use of opioids. Many health care providers and clients fear addiction when long-term opioid use is prescribed to manage pain, although this fear is often in-appropriate. Because of this concern, health care providers require opioid agreements and random urine testing in clients who require long-term opioid therapy. The effectiveness of agreements is lacking, and there are ethical concerns about using them for all clients who require long-term opi-oid therapy. This raises the question as to whether agreements protect clients or health care pro-viders.
Answer to Question 2
ANS: 1
Complete pain relief is not always achievable, but reducing pain to a tolerable level is realistic. Thus a primary nursing goal is to provide pain relief that allows clients to participate in their re-covery. Successful pain management does not necessarily mean pain elimination, but rather at-tainment of a mutually agreed-upon pain-relief goal that allows clients to control their pain in-stead of the pain controlling them. A person in pain feels distress or suffering and seeks relief. However, you as the nurse cannot see or feel the client's pain. It is realistic that the client will most likely experience postoperative pain. The nurse should not use a pain scale to compare the pain of one client to that of another client.