Answer to Question 1
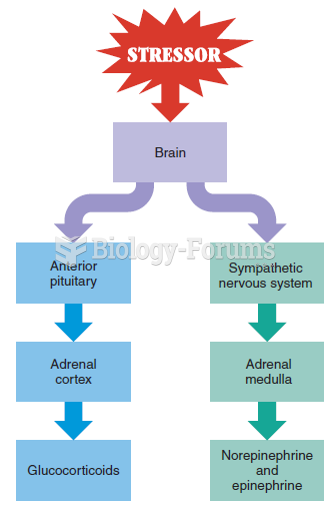
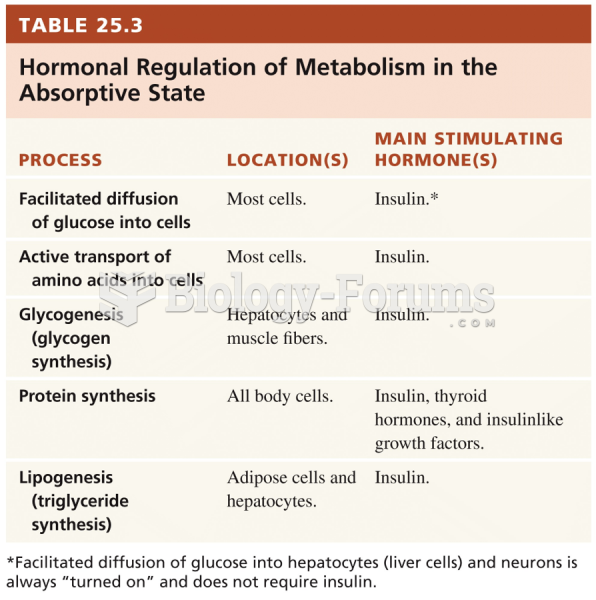
Due to this patient's recent traumatic event, his metabolism was greatly affected. Not only was he experiencing a local stress due to the gunshot wound and various injuries, but he was also experiencing a systemic metabolic response. Critical illness, serious infection, severe injury, burns, or severe psychological stress can initiate this metabolic response. Metabolic stress encompasses three phases: the ebb phase, acute flow phase, and recovery phase or adaptive flow phase. The ebb phase occurs within the first 24-48 hours and is characterized by hemodynamic instability. There is a period of severe shock with depression of enzymatic activity and oxygen consumption, resulting in decreased cardiac output, decreased core temperature, and increased lactic acidosis. It is critical during this time to conduct fluid resuscitation and oxygen delivery. Thus, feeding this patient while he is still hemodynamically unstable is not a top priority for this stage. During the acute flow phase, which occurs from 3 to 10 days after initial stress event, the body is hypermetabolic with increased cardiac rate and oxygen consumption. There is also an increase in glucose production via gluconeogenesis (with resulting hyperglycemia), variable lipolysis, and increased protein breakdown for a gluconeogenic substrate. The body uses more amino acids from this muscle breakdown to create precursors for acute-phase proteins and glutamine for gut metabolism. This causes an increase in protein mobilization, increased urinary nitrogen excretion, and lean body mass wasting. During this acute flow phase, the body is activating its survival mechanisms to maintain organ systems and promote healing. Unfortunately, this also increases the risk for malnutrition and further complications including loss of lean body mass . The goal of this stage is to minimize catabolism. During the last stage of recovery/adaptive flow phase, the acute flow phase subsides and the initiation of recovery and repair processes begins. This results in a decrease in energy and protein needs due to the decrease in inflammation and catabolism, while anabolism begins to occur. This third phase can last up to one year after initial injury.
Based on the information we have about this patient, he was admitted with symptoms of shock and was hemorrhaging and then progressed into the flow phase, as indicated by his high metabolic needs of 3657 kcal/day. Also, we can see that the metabolic stress continued for at least 7 days as indicated by his labs. The labs that indicate inflammationelevate d WBC, elevated CRP, and low albumin. The results of his urinalysis also indicate a catabolic state as well as uncontrolled hyperglycemia as he was spilling ketones and glucose into his urine. The presence of edema is due to third spacing of intravascular fluids and due to severe hypoalbuminemia.
Answer to Question 2
Gastric resection and repair could inhibit acid production (thus decreasing iron, calcium and vitamin B12 absorption), intrinsic factor secretion, change gastric motility, and reduce the amount of food he is able to eat at one time initially, but the stomach will adapt over a few months and he will return to normal function. Liver hemorrhage may disrupt liver functionmetabolism of fats, proteins, and carbohydrates as well as bile production and synthesis of albumin and clotting factorswhich will be noticeable in the lab values and nutritional status of the patient if function is not recovered. Resection of the proximal jejunum usually has very few long-term effects because the ileum compensates for the nutrient absorption of that part of the GI tract. The colon and ileum together absorb the increased fluid load and electrolyte load efficiently and the ileum continues to absorb bile salts so that they do not reach the colon to interfere with salt and water reabsorption.