Answer to Question 1
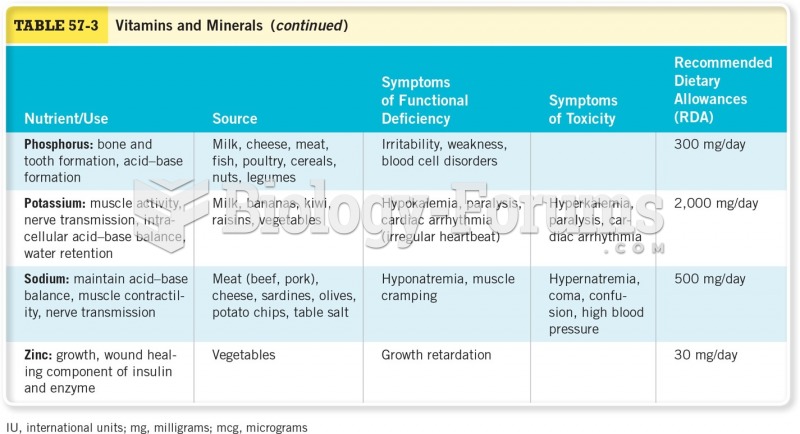
Unlike the organic vitamins, which are easily destroyed, minerals are inorganic elements that always retain their chemical identity. Once minerals enter the body, they remain there until excreted; they cannot be changed into anything else.
The minerals also differ from the vitamins in the amounts the body can absorb and in the extent to which they must be specially handled. Some minerals, such as potassium, are easily absorbed into the blood, transported freely, and readily excreted by the kidneys, much like the water-soluble vitamins. Other minerals, such as calcium, are more like fat-soluble vitamins in that they must have carriers to be absorbed and transported. And, like some of the fat-soluble vitamins, minerals consumed in excess can be toxic.
The bioavailability of minerals varies. Some foods contain binders that combine chemically with minerals, preventing their absorption and carrying them out of the body with other wastes. Examples of binders include phytates, which are found primarily in legumes, seeds, nuts, and grains, and oxalates, which are present in rhubarb, beet greens, sweet potatoes, and spinach, among other vegetables. These foods contain more minerals than the body actually receives for use.
The presence or absence of one vitamin can affect another's absorption, metabolism, and excretion. The same is true of the minerals. The interactions between sodium and calcium, for example, cause both to be excreted when sodium intakes are high. Phosphorus binds with magnesium in the GI tract, so magnesium absorption is limited when phosphorus intakes are high.
Answer to Question 2
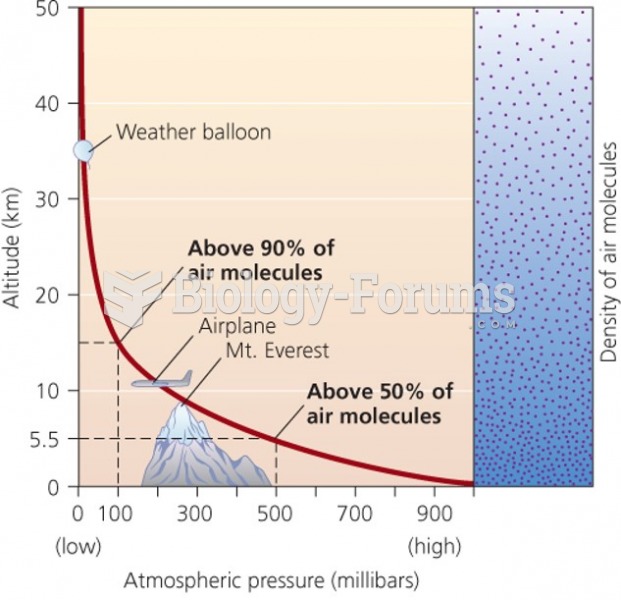
Whenever blood volume or blood pressure falls too low, or whenever the extracellular fluid becomes too concentrated, the hypothalamus signals the pituitary gland to release antidiuretic hormone (ADH). ADH is a water-conserving hormone that stimulates the kidneys to reabsorb water. Consequently, the more water you need, the less your kidneys excrete. These events also trigger thirst. Drinking water and retaining fluids raise the blood volume and dilute the concentrated fluids, thus helping to restore homeostasis.
Cells in the kidneys respond to low blood pressure by releasing an enzyme called renin. Through a complex series of events, renin causes the kidneys to reabsorb sodium. Sodium reabsorption, in turn, is always accompanied by water retention, which helps to raise blood volume and blood pressure.
In addition to its role in sodium retention, renin hydrolyzes a protein from the liver called angiotensinogen to angiotensin I. Angiotensin I is inactive until another enzyme converts it to its active formangiotensin II. Angiotensin II is a powerful vasoconstrictor that narrows the diameters of blood vessels, thereby raising the blood pressure.
In addition to acting as a vasoconstrictor, angiotensin II stimulates the release of the hormone aldosterone from the adrenal glands. Aldosterone signals the kidneys to excrete potassium and to retain more sodium, and therefore water, because when sodium moves, water follows. Again, the effect is that when more water is needed, less is excreted.