Answer to Question 1
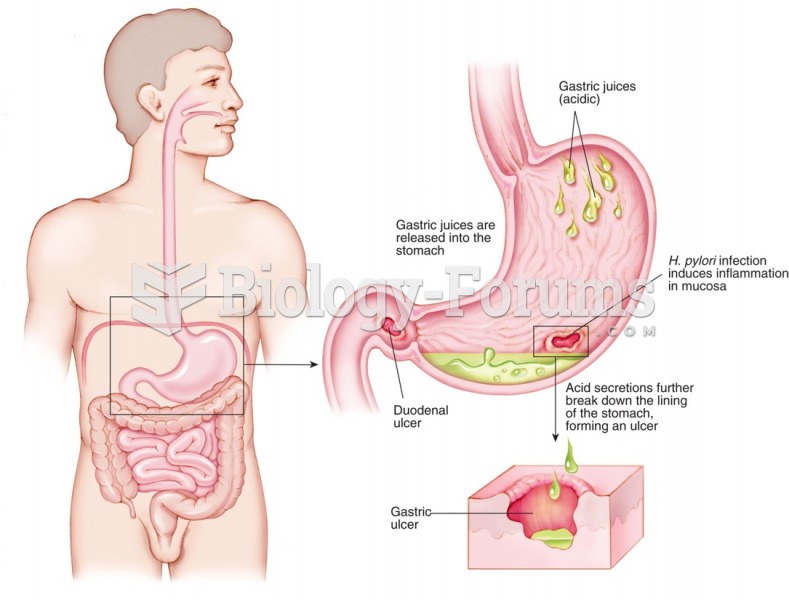
Helicobacter pylori is a microorganism whose only natural host is the human.
It is found primarily on the surface of the antrum of the stomach.
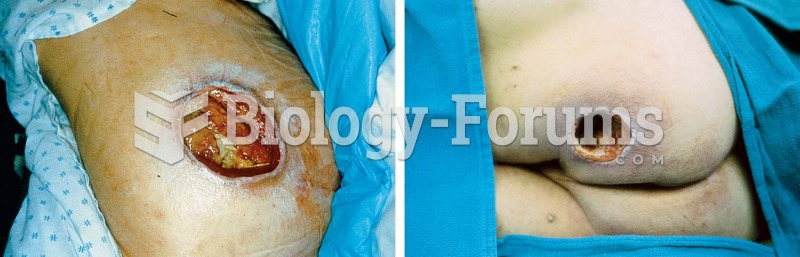
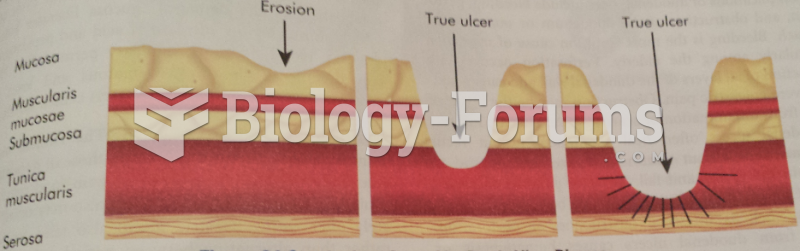
This microorganism has been established to be the most common cause of gastritis and it is estimated that 92 of duodenal ulcers and 70 of gastric ulcers are caused by H pylori.
By-products produced by the organism result in damage to the epithelium and impair the mucus barrier within the stomach.
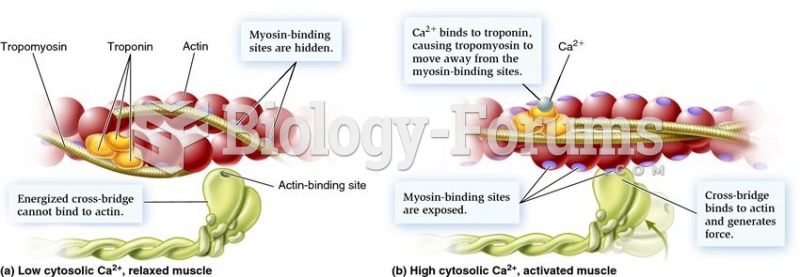
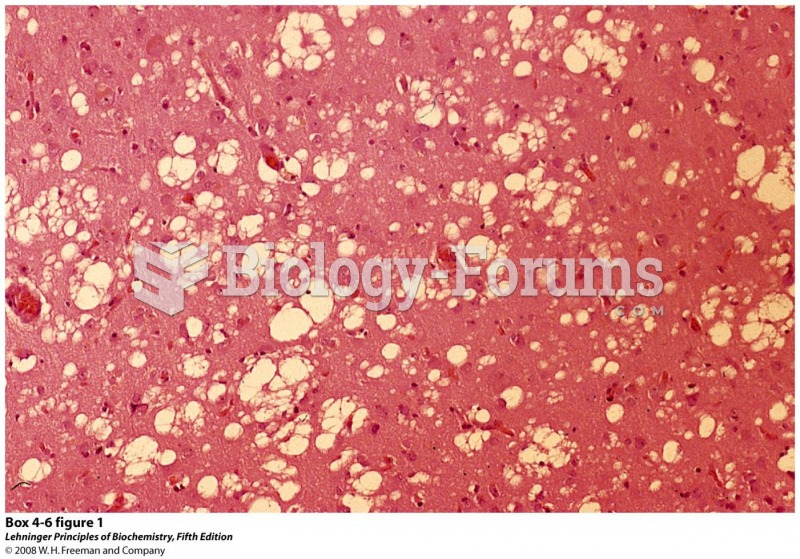
Helicobacter pylori, a spiral-shaped, flagellated, gram-negative rod, lives on the gastric mucosa under the mucous layer of the stomach and attaches to mucus-secreting cells that line the stomach. These organisms break down urea to produce ammonia, which helps to neutralize acid in the immediate vicinity of these bacteria and enhance their survival.
H. pylori organisms subsequently produce various proteins that damage mucosal cells. This damage attracts lymphocytes and causes persistent inflammation.
H. pylori can be identified in almost all patients with duodenal ulcers and in approximately 80 of patients with gastric ulcer in the absence of other precipitating factors such as NSAID use or hypersecretory conditions (e.g., Zollinger-Ellison syndrome).
Answer to Question 2
04/13/2015
A: 10 yo F, Olivia Foster
PMH: Spastic quadriplegic cerebral palsy, prematurity, developmental delay, seizure d/o, speech difficulties, GERD, constipation
PSH: ITB pump insertion (Aug 2013), multiple lower limb surgeries (2009-2012)
Meds: polyethylene glycol 3350 8 g bid, Lansoprazole 20 mg qd, baclofen 274 mcg/day, phenytoin 50 mg bid, pediatric gummy complete multivitamin bid
Appearance: thin, pale, dry skin, normal turgor, dry mucous membranes
Abdomen: soft, nontender, nondistended, BS present, ITB pump in lower L abdomen
Neuromuscular: hypertonia, mild to moderate contractures in upper/lower limbs. altered gait
Activity: recent fall, walks short distances w/crutches, wheelchair for long distances, GMFCS level 3
Labs: BUN 19, Protein 8, Albumin 5.1, ALP 625, 25-(OH)D 16
Diet: scrambled egg (w/Tbsp 1 milk), 6-8 oz water, 1/2 banana; 1/2 cup cooked carrots, 4-6 oz chocolate milk, 1/2 cup macaroni and cheese; 6 oz yogurt w/strawberries, 6-8 oz water; 1/2 cup rice and black bean casserole, 1/2 cup peaches, 4-6 oz 1 milk; 6-8 oz water, 1/2 cup apple sauce (1 tsp cinnamon sugar); sips water throughout day
Diet Hx: states can eat more if provided; advanced mechanical diet; vegetarian diet; somewhat picky (dislikes sweets); consistent eater in regards to portion sizes/mealtimes
Ht: 130.5 cm (10th percentile, z-score: -1.38) Wt: 23.1 kg (1st percentile; z-score: -2.35, down from -1.8 over the past year) BMI: 13.6 kg/m2 (2nd percentile; z-score: -2.07, down from -1.5 over the past year)
EER: 1800 kcal/d; EPR: 22 g/d; EFR:1562 mL/day
D: Inadequate oral intake related to oral motor dysfunction, limited food preferences, and need for prolonged feeding times as evidenced by reported energy intake of 60 estimated needs, BMI of < 3rdile and z-score of -2.07, and decrease in growth velocity over the past 2 years.
Altered nutrition related lab values (vitamin D) related to inadequate intake, increased vitamin D metabolism secondary to Phenytoin use, and decreased sunlight exposure as evidenced by 25-hydroxyvitamin D level(16 ng/mL) indicative of clinical deficiency.
I: Goal to meet caloric needs via power packing start by increasing energy intake by 10-20 daily until next follow up. Provide education to mom and pt on how to power pack meals based on food/beverages preferences.
Provide vitamin D supplementation of 400 IUs per day to normalize status. Take supplement with meals to enhance absorption as vitamin D is fat soluble.
M/E: Monitor weight, height, growth patterns (CDC charts), tolerance to increased caloric/fat intake.
Assess compliance with dietary intervention - intake, supplementation
Recheck serum 25-(OH)D level in 8 weeks.
Follow-up in 2-3 month to assure proper growth and adequacy of vitamin D supplementation.