Answer to Question 1
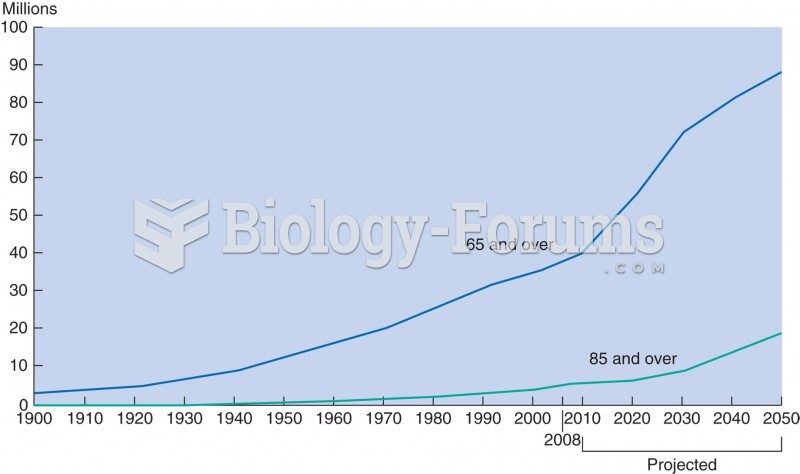
The Woman's Health Initiative study indicated that women who began HT after 60 years of age or later than 10 years after menopause had an increased risk for CHD. It is thought that these women began HT with the preliminary development of atherosclerosis; the use of therapeutic hormones accelerated inflammatory cytokine activity that led to unstable plaque formation and the development of symptoms. When corrected for age and the time when HT was implemented, the WHI demonstrated that younger women (under 60) and women who began HT within 10 years after menopause received the cardioprotective benefits of the treatment. The Nurses' Health Study confirmed that, if started shortly after menopause, HT reduced CHD by 30. Studies consistently show, however, an increased risk of thromboembolism in women using HT, particularly within the first 2 years of treatment.
It is thought that certain plant oils that contain substances similar to steroid hormones may be used as a natural supplement when human estrogen levels decline. Soy and red clover contain phytoestrogens, which are also said to exert estrogen effects in the body when taken as supplements. Although the use of these products has increased, their effectiveness has not yet been demonstrated in clinical trials.
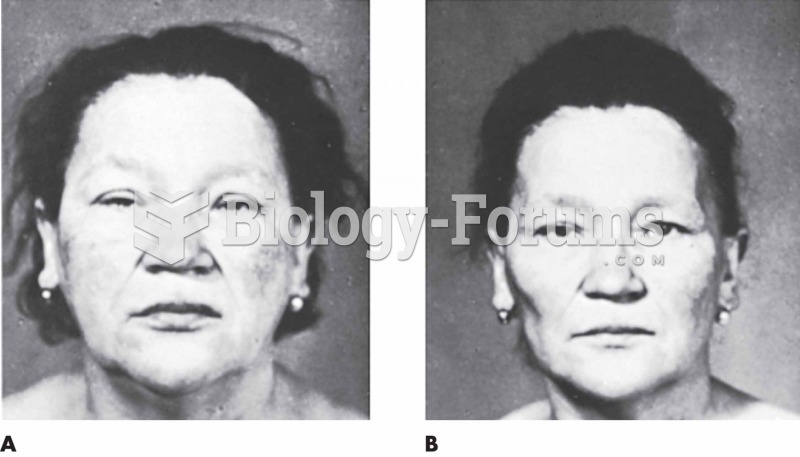
Declining estrogen levels have a variety of effects on the woman's reproductive organs. Subcutaneous fat declines and skin becomes less elastic, allowing the breasts to sag as tissue mass decreases. The ovaries, uterus, and cervix atrophy when not supported by estrogen. The production of cervical mucus also declines, leaving the vagina dry and prone to infection.
During puberty, estrogen is responsible for the accelerated growth of long bones and for initiating the closure of the epiphyseal plates. Estrogens also have the effect of antagonizing the actions of PTH; when estrogen declines in menopause, bone resorption accelerates. Women are therefore at an increased risk for osteoporosis after menopause.
Answer to Question 2
Cervical cancer is associated with certain HPV types, many of which are spread by sexual contact. The rate of cervical cancer is higher among women who have had sexual intercourse at an early age, have multiple sexual partners, or are in relationships with promiscuous men.
The Pap test involves the removal of a cell sample from the transitional zone and endocervix. The presence of cellular dysplasia is important as cervical cancer arises from the precursor lesions identified with the Pap smear. The CIN 3 (HSIL) indicates the presence of a high-grade squamous intraepithelial lesion and cervical cancer in situ.
The transformation zone is the area residing between the exocervix and endocervix. The exocervix is covered with stratified squamous epithelium and the endocervix by columnar epithelium. Because the transformation zone exists between these two areas, it consists of a functional squamocolumnar cellular region. Cervical cancer arises in the transformation zone because of its vulnerability during metaplasia. Genetic mutations, when the tissue is exposed to carcinogens, are more likely when the transformation zone is undergoing normal growth and cellular change.
The LEEP procedure involves the removal of cervical tissue using a thin, wire loop electrode. The electrical current allows the practitioner to cut the tissue sample and encourage coagulation at the site. The procedure can remove the entire transformational area to ensure the elimination of abnormal cells and for further histological evaluation.