Answer to Question 1
PFTs are performed initially, then 15 minutes after inhalation of a beta agonist. This is called a prepost
dilator study and is meant to determine whether a person has asthma. If L.B. has asthma, the
postdilator maneuver will show more than 15 improvement in airflow.
Describe the basic pathophysiology of asthma and provide an overview of its management.
Explain what each medication is, why she is taking it, and its appropriate use.
Demonstrate PFM and metered-dose inhaler (MDI) technique and ask for a return demonstration.
Teach her to identify and avoid triggers as much as possible. A journal or smartphone application
may assist with this. She needs to track seasonal symptoms and symptoms related to temperature,
humidity, dust, animal dander, pollen, perfume, and so on.
Make certain she has a written plan to treat exacerbations and knows when to seek emergency
assistance.
There are varying degrees of asthma. Individuals with mild persistent asthma typically have
symptoms that occur more than twice a week but less than once a day. Nighttime symptoms occur
more frequently than twice a month. L.B. may experience exacerbations that might affect activity,
but her normal physical activity should not be affected.
Asthma is an inflammatory disease, and triamcinolone is an anti-inflammatory drug. The goal of
treatment for mild asthma is to identify triggers, control inflammation with an anti-inflammatory,
and control secondary wheezing with a beta2 agonist (albuterol). Albuterol is a bronchodilator that
relaxes smooth muscles around the large airways. The albuterol MDI has fewer side effects than oral
medication, but she might experience some anxiety, heart palpitations, or slight tremors. These
symptoms can be worse if the MDI is not used correctly. You would review the proper use of the MDI.
Answer: a
Because the inhalation route delivers the drug directly to the lungs, lower drug doses are possible
and there are fewer systemic side effects. Unfortunately, there is considerable expense involved
with some inhalers and more manual dexterity is required to master an inhaler or other devices. Any
medication currently prescribed for asthma is not curative but used only to control symptoms.
A PFM is a hand-held device that measures the maximum flow rate that can be generated when an
individual takes a maximum inspiration then expels the volume with a maximum expiratory effort
through the PFM device.
Breathe in as deeply as you can, place the PFM in your mouth, and blow as hard and fast as you can.
Record the reading. Repeat two times for a total of three measurements. Remember that the PFM
reading is effort dependent and it is important for the readings to be within 5 of one another. If
one reading is much smaller than the other two, it should be discarded and another reading taken.
A decreased peak expiratory flow rate (PEFR) indicates airway obstruction. The maneuver requires a
consistent maximal effort on the part of the individual being tested.
The PEFR, measured in liters per minute, indicates airflow and is used to detect the presence of any
airflow obstruction. Normal PEFRs are based on height, age, and gender. PEFRs are used to monitor
the effect of medication and can detect a worsening condition before symptoms are apparent to the
individual. PEFR should be completed before and after inhaled medications for 2 weeks to develop
a personal best or goal. The provider then calculates 80 and 50 of the patient's personal best
and marks the meter with a green zone (which equals 80 to 100 of the personal best), yellow
zone (50 to 79), and red zone (below 50). Readings in the green zone indicate that the patient
is okay and may continue with daily activities. It is important that each patient have a care plan to
address what to do if the readings fall in the yellow or red zone. Readings in the yellow zone indicate
the patient is having a moderate asthma attack and should follow the plan for increasing airflow
rate. Readings in the red zone indicate the patient is having a severe asthma attack and should seek
immediate medical assistance.
If the PEFR is within the yellow zone, it indicates caution. Something is triggering the patient's
asthma, such as a cold or infection. A temporary increase in medications, such as use of a beta2-
adrenergic agonist inhaler more frequently, might be needed to increase airflow.
If the PEFR is in the red zone, it indicates a serious problem and action must be taken. A typical
rescue plan consists of two to four puffs of a short-acting inhaled beta2-adrenergic agonist for up
to three treatments at 20-minute intervals or a single nebulizer treatment. The patient needs to
contact or be seen by the health care provider. Depending on symptoms, oral corticosteroids may
be indicated.
Answer to Question 2
VS: Respiratory effort, respiratory rate, and oximetry to evaluate respiratory function.
Ear, nose, and throat (ENT): Because of the correlation between asthma and allergic rhinitis, observe
for findings associated with allergic rhinitis including pale, boggy turbinates, serous otitis, and
mucous drainage in the posterior pharynx.
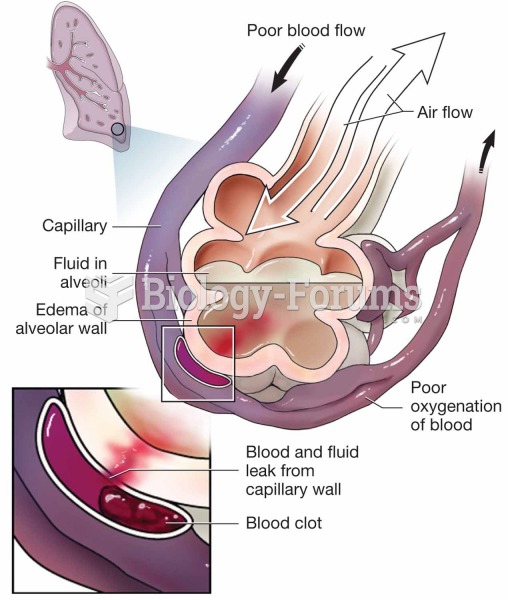
Lung sounds: Often wheezing is heard, but breath sounds may be clear. If the patient's airways are
very constricted, treatment with a beta agonist may relax the airways enough for wheezing to
be heard. Patients with chronic obstructive pulmonary disease (COPD) often have distant breath
sounds; patients with pneumonia may have crackles, wheezes, and egophony.
Lymph node palpation: To determine if an infection of the upper respiratory tract may be responsible
for her symptoms.
Abdominal palpation: Look for gastric tenderness that often accompanies gastroesophageal reflux
disease (GERD), which is a frequent asthma trigger.
Skin: Eczema can be an atopic manifestation of asthma.