Answer to Question 1
Although there has been a slight decline in heart rate and temperature and a slight increase in
oxygen saturation, M.N.'s vital signs are still abnormal and reflect that she has possibly developed
atelectasis or another pulmonary complication.
Following SBAR, you would first need to identify yourself and the patient. Then you would describe
the situation, focusing on the Spo2 of 88 and describing the earlier assessment findings: 118, 24,
101 F; auscultated decreased breath sounds and crackles in the right base posteriorly; right middle
and lower lobes percussed slightly dull; without productive cough, chest pain, or any anxiety.
You state how many hours postoperative the patient is; review the interventions you performed,
including pain medications given, ambulation efforts, and the use of IS and coughing and deep
breathing; and review the current status of the patient. You would conclude your remarks with the
belief that atelectasis is present and the recommendation that a chest x-ray (CXR) examination is
needed.
No. You should continue your plans and monitor effectiveness.
If M.N. had pneumonia, you would anticipate the physician ordering blood cultures, starting
breathing treatments, and initiating antibiotic therapy.
M.N.'s sister and perhaps M.N. are concerned that something might have gone wrong with M.N.
during her hospitalization. State everything in positive terms because they need reassurance. Inform
them that M.N. was very sick when she was admitted and that her incision site is painful. Explain
that you are giving M.N. pain medication so that she will be able to cough and breathe deeply, move
around in bed, and walk so that she will not develop pneumonia. Assure them that M.N. is recovering
well from surgery. Show M.N.'s sister how to help M.N. with ambulation and coughing.
Answer to Question 2
M.N. appears to be developing atelectasis. She has the common presenting symptoms of dyspnea
and hypoxia, accompanied by fever, crackles, and diminished breath sounds. Pneumonia typically
does not occur this early; the common signs of pulmonary embolism M.N. does not have include
anxiety, pleuritic chest pain, cyanosis, and hypoxia.
The effects of anesthesia, reluctance to cough and deep breathe because of inadequate pain control
and location of the surgical incision, and immobility contribute to the inadequate lung expansion
that predisposes patients to developing atelectasis.
The nursing priority right now is to improve M.N.'s respiratory status.
Apply the oxygen per protocol because her Spo2 is below 95.
Elevate the head of her bed.
Administer pain medication if the time interval is appropriate. Tell her that you are going to let her
rest for 20 minutes until the morphine has had time to take effect; then you will be back to help her
dangle, use the incentive spirometer (IS), and cough and deep breathe.
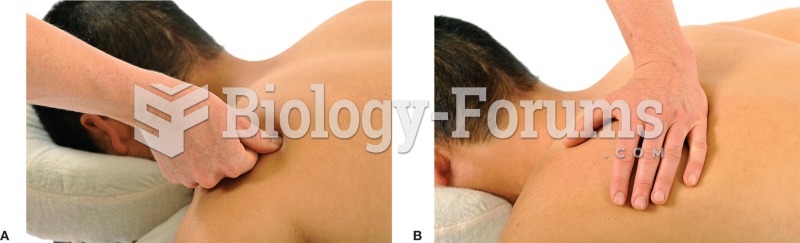
Have her cough and deep breathe every hour, splinting her incision. If needed, review with her
appropriate technique and coach her while she coughs.
Explain and demonstrate the correct use of the IS. Have her use the IS every hour while awake.
Have her dangle on the side of the bed as ordered.
Turn and reposition every 2 hours.
Reassess her vital signs every 2 hours and monitor for signs of deterioration.
Be prepared to call a physician if her condition worsens.
Answers: a, c, d, e
To prevent pulmonary complications, patients should be encouraged to cough and deep breathe,
ambulate as soon as possible, and splint the incision to minimize discomfort during activity. For
patient safety, the nurse should enlist the assistance of other staff members, including the NAP,
during these efforts, while encouraging the patient to help. The NAP cannot instruct the patient on
the use of the IS; teaching is the responsibility of the registered nurse (RN); however, the NAP could
reinforce teaching provided by the RN. The NAP can take the patient's vital signs as long as the
RN has given the NAP parameters that the NAP would need to report to the RN. Auscultating lung
sounds is not within the scope of practice for the NAP.
Decreased resting respiratory rate
Increased breath sounds over the right lower lobe by auscultation
Crackles clearing or clear lung sounds
Spo2 greater than 90
Afebrile status
Resonant percussion