|
|
|
Bacteria have been found alive in a lake buried one half mile under ice in Antarctica.
Your chance of developing a kidney stone is 1 in 10. In recent years, approximately 3.7 million people in the United States were diagnosed with a kidney disease.
As many as 28% of hospitalized patients requiring mechanical ventilators to help them breathe (for more than 48 hours) will develop ventilator-associated pneumonia. Current therapy involves intravenous antibiotics, but new antibiotics that can be inhaled (and more directly treat the infection) are being developed.
The average office desk has 400 times more bacteria on it than a toilet.
In 1885, the Lloyd Manufacturing Company of Albany, New York, promoted and sold "Cocaine Toothache Drops" at 15 cents per bottle! In 1914, the Harrison Narcotic Act brought the sale and distribution of this drug under federal control.
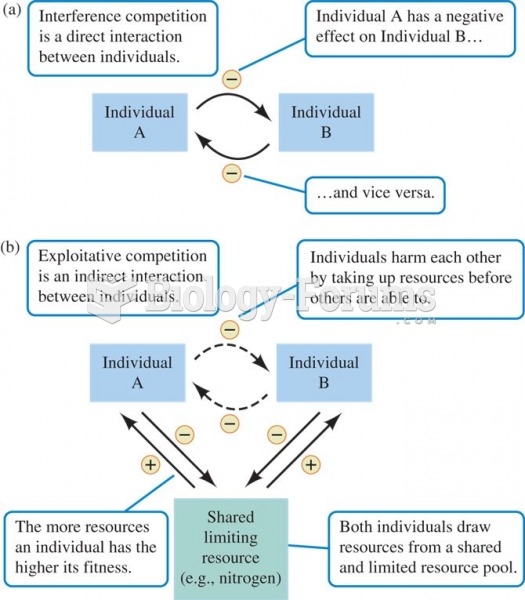 Competition can be (a) direct, or (b) indirect interaction among individuals of the same or differen
Competition can be (a) direct, or (b) indirect interaction among individuals of the same or differen
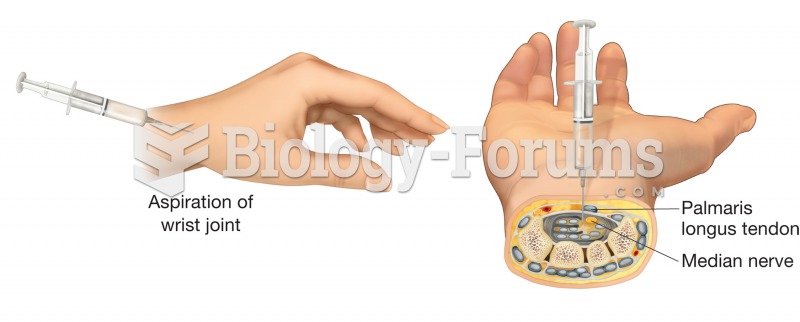 Arthrocentesis. The aspiration of fluid is a common treatment for joint injuries resulting in inflam
Arthrocentesis. The aspiration of fluid is a common treatment for joint injuries resulting in inflam
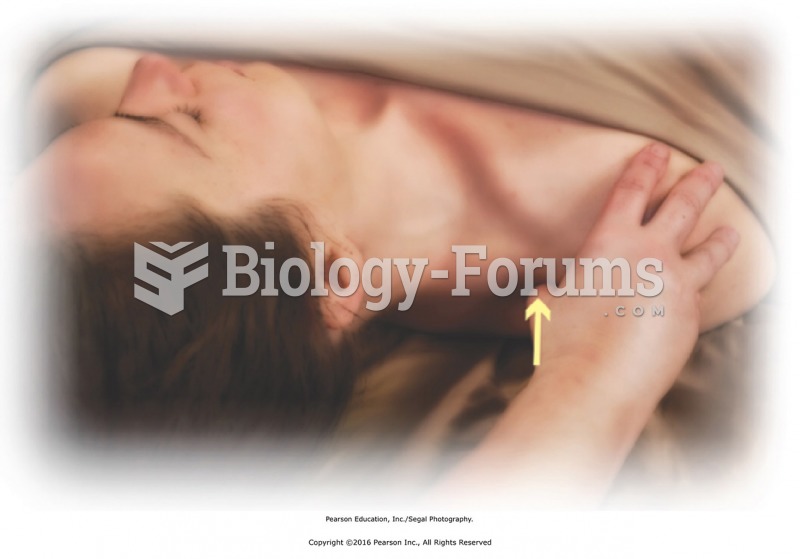 Apply direct pressure along upper trapezius, turning the head to access the area. Use your thumb to ...
Apply direct pressure along upper trapezius, turning the head to access the area. Use your thumb to ...