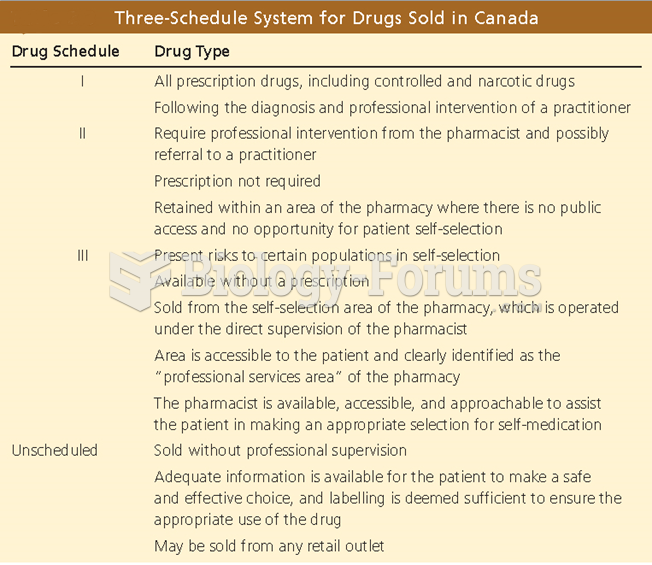
Prescription management represents a high level of risk when the patient's presenting problem is complicated by a chronic condition with any progression.
Read the following medical documentation then answer the following five questions.
CC: Diarrhea
HPI: 68-year-old male presents to the emergency department with a four-day history of loose stools. Patient states that over the past several days he has had at least six to 10 loose, watery stools per day. No hematochezia or melena. He denies any fever or abdominal pain. No chest pain, shortness of breath, or peripheral edema. Did see his primary care physician several days ago, who increased his metoprolol to 100 mg daily.
PMH:
1. Coronary artery disease, status post CABG 2002
2. Sternal osteomyelitis, status post CABG
3. Gout
4. Chronic renal insufficiency, baseline creatinine 2.0
5. Ischemic cardiomyopathy, last echocardiogram 5/21/2012, EF 32
6. Peripheral neuropathy
7. Diabetes mellitus, type II (noninsulin dependent)
8. Hypertension
9. Appendiceal abscess, hospitalized 3/2010 to 4/2010, treated by conservative medical management only
10. Mild COPD
ROS: As per HPI.
Medications:
1. Metoprolol ER 100 mg by mouth daily (dose increased three days ago)
2. Amitriptiline 25 mg by mouth at night
3. Plavix 75 mg by mouth daily
4. Aspirin 81 mg by mouth daily
5. Lisinopril 20 mg by mouth daily
6. Spirinolactone 25 mg by mouth daily
7. Lasix 40 mg by mouth daily
8. Colchicine 0.6 mg by mouth daily
9. Simvistatin 20 mg by mouth every night
10. Glipizide 10 mg by mouth daily
PE:
Vital signs: Temp 37.2 HR 32 RR 14 BP 112/61 SaO2 99 at room air
General: Alert, thin male seated in hospital gurney, no acute distress.
NEURO: Cranial nerves II-XII intact. Alert, oriented times three.
HEENT: PERRL, EOMI. Sclera nonicteric. Mucus membranes moist. Neck supple, no adenopathy.
PULM: Lungs clear to auscultation bilaterally.
CARD: Bradycardic, regular rhythm, distant heart sounds. Well-healed sternotomy scar noted.
ABD: Soft, nontender, nondistended. No masses palpable. Bowel sounds present.
EXT: Warm, well perfused, no edema.
ECG: Sinus bradycardia, with peaked T waves and widened QRS noted. No ST depressions. Poor R wave progression.
Laboratory:
CBC normal
Comprehensive metabolic panel: significant for sodium 122, potassium 6.7, chloride 96, bicarbinate 12, BUN 101, creatinine 4.0.
Impression: 68-year-old male with acute renal failure and secondary metabolic acidosis with hyperkalemia and bradycardia
Plan:
1. NEURO: No issues.
2. CARDIO: Bradycardia is likely secondary to hyperkalemia, but may also be from recent increase in metoprolol. Give calcium gluconate stat, monitor cardiac function carefully as potassium is corrected. Hold lisinopril and metoprolol for now. Gentle hydration in light of ischemic cardiomyopathy and depressed ejection fraction.
3. PULM: No current issues. Continue Duonebs TID.
4. FEN/GI: Watery diarrhea ongoing. Likely viral, but will send stool culture, c. diff (in light of extended hospitalizations). Diabetic, low salt diet. D50/Insulin/Kayexelate/Albuterol nebs. Recheck potassium in two hours.
5. RENAL: Acute failure, likely secondary to dehydration from diarrhea. Hold lisinopril, gentle fluid hydration overnight. Follow function.
6. ENDO: Hold glypizide for now, cover with regular insulin sliding scale.
7. HEME: No issues.
8. ID: No antibiotics for now, await results from stool studies.
Indicate whether this statement is true or false.
Question 2
The performed ECG supports a moderate level of risk in the diagnostic procedure ordered portion of the table of risk.
Read the following medical documentation then answer the following five questions.
CC: Diarrhea
HPI: 68-year-old male presents to the emergency department with a four-day history of loose stools. Patient states that over the past several days he has had at least six to 10 loose, watery stools per day. No hematochezia or melena. He denies any fever or abdominal pain. No chest pain, shortness of breath, or peripheral edema. Did see his primary care physician several days ago, who increased his metoprolol to 100 mg daily.
PMH:
1. Coronary artery disease, status post CABG 2002
2. Sternal osteomyelitis, status post CABG
3. Gout
4. Chronic renal insufficiency, baseline creatinine 2.0
5. Ischemic cardiomyopathy, last echocardiogram 5/21/2012, EF 32
6. Peripheral neuropathy
7. Diabetes mellitus, type II (noninsulin dependent)
8. Hypertension
9. Appendiceal abscess, hospitalized 3/2010 to 4/2010, treated by conservative medical management only
10. Mild COPD
ROS: As per HPI.
Medications:
1. Metoprolol ER 100 mg by mouth daily (dose increased three days ago)
2. Amitriptiline 25 mg by mouth at night
3. Plavix 75 mg by mouth daily
4. Aspirin 81 mg by mouth daily
5. Lisinopril 20 mg by mouth daily
6. Spirinolactone 25 mg by mouth daily
7. Lasix 40 mg by mouth daily
8. Colchicine 0.6 mg by mouth daily
9. Simvistatin 20 mg by mouth every night
10. Glipizide 10 mg by mouth daily
PE:
Vital signs: Temp 37.2 HR 32 RR 14 BP 112/61 SaO2 99 at room air
General: Alert, thin male seated in hospital gurney, no acute distress.
NEURO: Cranial nerves II-XII intact. Alert, oriented times three.
HEENT: PERRL, EOMI. Sclera nonicteric. Mucus membranes moist. Neck supple, no adenopathy.
PULM: Lungs clear to auscultation bilaterally.
CARD: Bradycardic, regular rhythm, distant heart sounds. Well-healed sternotomy scar noted.
ABD: Soft, nontender, nondistended. No masses palpable. Bowel sounds present.
EXT: Warm, well perfused, no edema.
ECG: Sinus bradycardia, with peaked T waves and widened QRS noted. No ST depressions. Poor R wave progression.
Laboratory:
CBC normal
Comprehensive metabolic panel: significant for sodium 122, potassium 6.7, chloride 96, bicarbinate 12, BUN 101, creatinine 4.0.
Impression: 68-year-old male with acute renal failure and secondary metabolic acidosis with hyperkalemia and bradycardia
Plan:
1. NEURO: No issues.
2. CARDIO: Bradycardia is likely secondary to hyperkalemia, but may also be from recent increase in metoprolol. Give calcium gluconate stat, monitor cardiac function carefully as potassium is corrected. Hold lisinopril and metoprolol for now. Gentle hydration in light of ischemic cardiomyopathy and depressed ejection fraction.
3. PULM: No current issues. Continue Duonebs TID.
4. FEN/GI: Watery diarrhea ongoing. Likely viral, but will send stool culture, c. diff (in light of extended hospitalizations). Diabetic, low salt diet. D50/Insulin/Kayexelate/Albuterol nebs. Recheck potassium in two hours.
5. RENAL: Acute failure, likely secondary to dehydration from diarrhea. Hold lisinopril, gentle fluid hydration overnight. Follow function.
6. ENDO: Hold glypizide for now, cover with regular insulin sliding scale.
7. HEME: No issues.
8. ID: No antibiotics for now, await results from stool studies.
Indicate whether this statement is true or false.