Answer to Question 1
C
Answer to Question 2
The following stages identified by Dr. Elisabeth Kbler-Ross have been found to be a valuable paradigm in understanding a terminally ill person's behavior:
Stage 1: Denial. It can't be. No, not me. There must be a mistake. This is generally the first reaction when a person learns she or he has a terminal illness. Dr. Kbler-Ross believes such a reaction is functional because it helps cushion the impact that death will soon be inevitable.
Stage 2: Rage and anger. Why me Look at the good things I've done and still need to do for the members of my family. This just isn't fair Patients resent the fact that they will soon die while others remain healthy and alive. God is frequently a special target of the anger during this stage, as God is viewed as unfairly imposing a death sentence. Dr. Kbler-Ross believes that such anger is inevitable, and that the patient should be allowed to express such anger. And she adds, God can take it. During this stage, family and hospital staff frequently experience difficulty in coping with the anger, which is displaced in many directions. The patient may charge that the doctor is incompetent, that the hospital surroundings are inhumane, that the nurses are unconcerned about people, that there is too much noise, and so on. The underlying reasons generating the patient's anger need to be remembered during this stage. Reacting personally or angrily to the patient's anger will only feed into that hostile behavior. During this stage, conveying to the patient that she or he is an important person who is worthy of respect, time, and understanding will usually lead to a reduction of angry demands.
Stage 3: Bargaining. I realize my death is inevitable, but if I could just live 6 months more I could During this stage, patients come to accept their terminal illness but try to strike bargains (frequently with God) for more time. They promise to do something worthwhile or to be good in exchange for another month or year of life. Dr. Kbler-Ross indicates that even agnostics and atheists sometimes attempt to bargain with God during this stage.
Stage 4: Depression. Yes, it will soon be over. It's really sad, but true. The first phase of this stage is when the patient mourns things not done, past losses, and wrongs committed. This type of depression is frequently exacerbated by guilt or shame about acts of omission or commission. Counseling during this phase generally focuses on helping the patient to resolve feelings of guilt and shame. In some cases, this may involve helping family members to make realistic plans for their future and to reassure the patient that vital unfinished situations are being taken care of. The second phase of this stage is when the patient enters a state of preparatory grief, in which she or he is getting ready for the inevitable by taking into account impending losses. During this stage, the patient should not be encouraged to be cheerful; this would interfere with the necessity for the patient to contemplate his or her impending death. During this phase, the patient generally becomes quiet and does not want to see visitors. The patient is in the process of losing everything and everybody she or he loves. If the patient is allowed to express this sorrow, final acceptance of death will be much easier. In addition, the patient will be grateful to those who are able to sit quietly nearby, without telling him or her not to be sad. According to Dr. Kbler-Ross, when a dying patient no longer continues to request to see someone to discuss his or her situation, it is a sign that unfinished business is completed and the patient has reached the final stage.
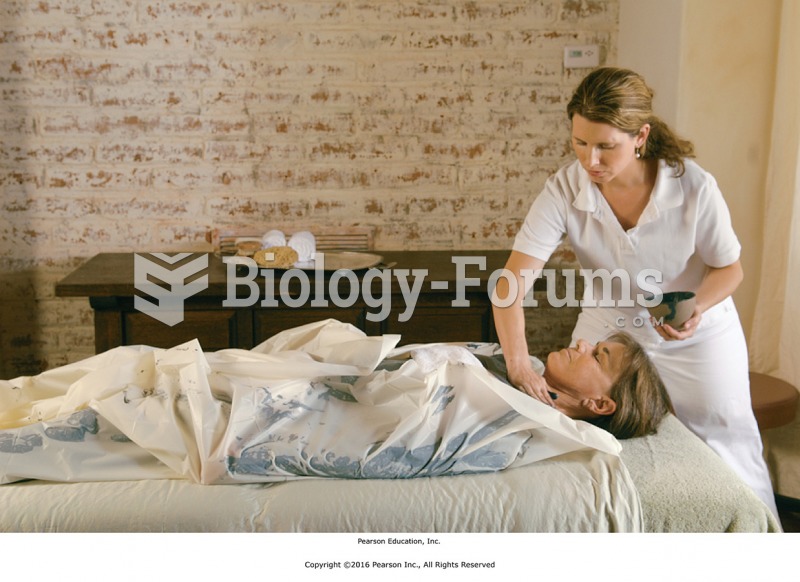
Stage 5: Acceptance. I will soon pass on, and it's all right. Dr. Kbler-Ross describes this final stage as not a happy stage, but neither is it unhappy. It's devoid of feelings but it's not resignation; it's really a victory. During this stage, visitors often are not desired because the patient no longer is in a talkative mood. Communications with a counselor may become more nonverbal than verbal. Patients may just want to hold the counselor's hand-to sit together in silence with someone who is comfortable in the presence of a dying person.
Dr. Kbler-Ross notes that some patients continue grieving about their terminal illness without ever reaching the final stage of acceptance. She also notes that not everyone will progress through these stages as presented here. There is often considerable movement back and forth among stages. For example, a patient may go from denial to depression, to rage and anger, back to denial, then to bargaining, then to depression, and so on.