This topic contains a solution. Click here to go to the answer
|
|
|
Did you know?
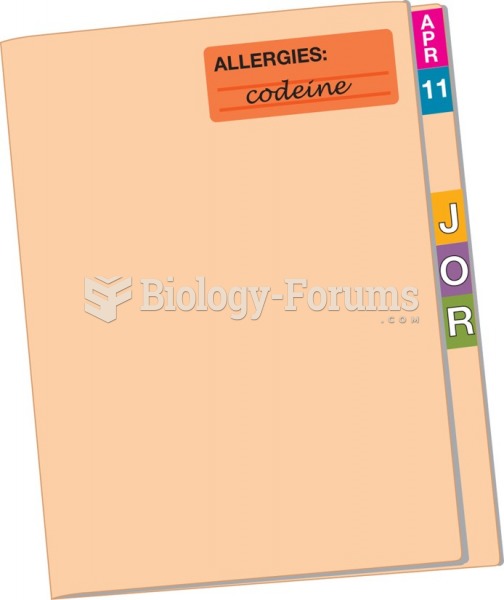
More than 34,000 trademarked medication names and more than 10,000 generic medication names are in use in the United States.
Did you know?
People with high total cholesterol have about two times the risk for heart disease as people with ideal levels.
Did you know?
According to the CDC, approximately 31.7% of the U.S. population has high low-density lipoprotein (LDL) or "bad cholesterol" levels.
Did you know?
Critical care patients are twice as likely to receive the wrong medication. Of these errors, 20% are life-threatening, and 42% require additional life-sustaining treatments.
Did you know?
The first documented use of surgical anesthesia in the United States was in Connecticut in 1844.