Answer to Question 1
Answer:
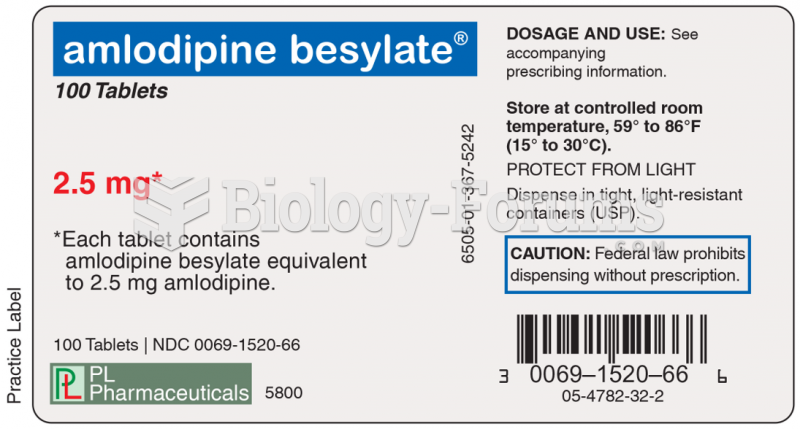
a. A valid claim form must be on file showing the eligible diagnosis for which the drugs are being prescribed. This form shows that the patient was under the care of a physician for the covered diagnosis when the prescription was issued. After a valid claim form has been accepted, it is not necessary for a new claim form to accompany each drug claim as long as the patient is still under the doctor's care and the diagnosis is still valid. For example, if the diagnosis is of a chronic nature, drugs will often be refills of earlier prescriptions.
b. The pharmacy bill, receipt, or pharmacy statement for each prescription must accompany the request for payment.
c. All drug receipts or pharmacy bills must show the prescription number, the name of the physician, the name of the patient, the date of issuance, and the amount charged. If any of these items are omitted, the validity of the prescription should be checked prior to payment of the claim. Some receipts may also list the type of drug. This is helpful for determining whether the drug is a prescription drug or an over-the-counter drug.
d. The drugs must be appropriate for the condition being treated, the amount of time since the first diagnosis of the condition, and the amount of drug prescribed. For example, persons suffering from a serious heart disease or diabetes may require large amounts of drugs over an extended period of time, whereas a patient suffering from an ear infection would require a small amount of drugs over a much shorter period of time.
e. If prescriptions are questionable, further information should be obtained from the prescribing physician, not from the patient.
Answer to Question 2
Answer:
a. Fully analyze the claim initially. Consider all possible reasons for acceptance or denial. Look for a way to pay a claim, not deny it. Often an initial review of a claim will reveal clear and obvious grounds for denial. Sometimes the obvious grounds disappear later when the denial is questioned. Always clearly document the grounds for denial. Resist the natural temptation to deny a claim without a complete investigation and without considering all other possible grounds for acceptance. Keep in mind that for health plan years beginning on or after September 23, 2010, the Affordable Care Act of 2010 makes it illegal for insurance companies to rescind coverage based on an error or technicality.
b. Thoroughly investigate and document the facts within the claim file. This may be one of the most important steps that each examiner needs to take before paying or denying a claim. The lack of a proper investigation or documentation has probably resulted in more bad faith lawsuits than any other individual factor.
c. Handle claims promptly and keep claimants informed.
1. Give priority to delayed/pended claims.
2. Resolve conflicting evidence or information promptly.
3. Do not withhold or delay payments in hope of a compromise.
4. Be sure to indicate the date and other documentation for the following: when claims are received or processed, when correspondence is received or sent, and when telephone calls are received or made.
d. Make proper use of medical evidence.
1. Always contact the doctor to clear up any medical questions concerning the claimant.
2. When a second medical opinion is required, the proper selection of an independent medical examiner is very important. A specialist should be chosen for the specific disease or injury. The specialist must always be provided with all the claimant's relevant medical information and records, whether they are favorable or unfavorable. Also, the examiner cannot provide a correct conclusion unless the correct questions are asked. Sometimes asking the correct questions is the most difficult part of preparing a case for review.
e. Be observant in looking for excessive charges. There may be providers who indicate a long list of diagnoses to match the wide variety of tests given, so that the claim will be covered by the insurance carrier.