Answer to Question 1
The human body needs fatty acids, and it can make all but two of themlinoleic acid (the 18-carbon omega-6 fatty acid) and linolenic acid (the 18-carbon omega-3 fatty acid). These two fatty acids must be sup- plied by the diet and are therefore essential fatty acids. The cells do not possess the enzymes to make any of the omega-6 or omega-3 fatty acids from scratch, nor can they convert an omega-6 fatty acid to an omega-3 fatty acid or vice versa. Cells can, however, use the 18-carbon member of an omega family from the diet to make the longer fatty acids of that family by forming double bonds (desaturation) and lengthening the chain two carbons at a time (elongation). This is a slow process because the omega-3 and omega-6 families compete for the same enzymes. Too much of a fatty acid from one family can create a deficiency of the other family's longer fatty acids, which becomes critical only when the diet fails to deliver adequate supplies. Therefore, the most effective way to maintain body supplies of all the omega-6 and omega-3 fatty acids is to obtain them directly from foodsmost notably, from vegetable oils, seeds, nuts, fish, and other seafoods.
Most diets in the United States and Canada meet the minimum essential fatty acid requirement adequately. Historically, deficiencies have developed only in infants and young children who have been fed fat-free milk and low-fat diets or in hospital clients who have been mistakenly fed formulas that provided no polyunsaturated fatty acids for long periods of time. Classic deficiency symptoms include growth retardation, reproductive failure, skin lesions, kidney and liver disorders, and subtle neurological and visual problems.
Answer to Question 2
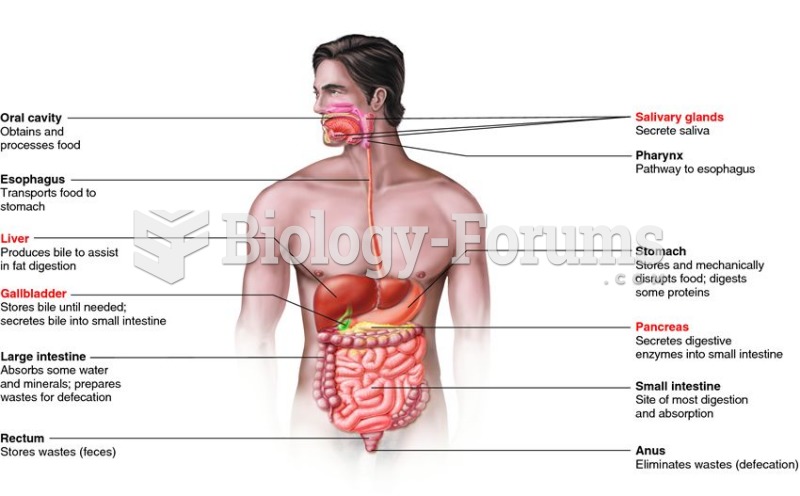
The chylomicrons are the largest and least dense of the lipoproteins. They transport diet-derived lipids (mostly triglycerides) from the small intestine (via the lymph system) to the rest of the body. Cells all over the body remove triglycerides from the chylomicrons as they pass by, so the chylomicrons get smaller and smaller. Within 14 hours after absorption, most of the triglycerides have been depleted, and only a few remnants of protein, cholesterol, and phospholipid remain. Special protein receptors on the membranes of the liver cells recognize and remove these chylomicron remnants from the blood.
Meanwhile, in the liverthe most active site of lipid synthesiscells are making cholesterol, fatty acids, and other lipid compounds. Ultimately, the lipids made in the liver and those collected from chylomicron remnants are packaged with proteins as a VLDL (very-low-density lipoprotein) and shipped to other parts of the body. As the VLDL travel through the body, cells remove triglycerides. As they lose triglycerides, the VLDL shrink and the proportion of lipids shifts. Cholesterol becomes the predominant lipid, and the lipoprotein becomes smaller and denser. As this occurs, the VLDL becomes an LDL (low-density lipoprotein), loaded with cholesterol, but containing relatively few triglycerides.
The LDL circulate throughout the body, making their contents available to the cells of all tissuesmuscles (including the heart muscle), fat stores, the mammary glands, and others. The cells take triglycerides, cholesterol, and phospholipids to use for energy, make hormones or other compounds, or build new membranes. Special LDL receptors on the liver cells play a crucial role in the control of blood cholesterol concentrations by removing LDL from circulation.
The liver makes HDL (high-density lipoprotein) to remove cholesterol from the cells and carry it back to the liver for recycling or disposal. By efficiently clearing cholesterol, HDL lowers the risk of heart disease. In addition, HDL have anti-inflammatory properties that seem to keep artery-clogging plaque from breaking apart and causing heart attacks