Answer to Question 1
To prepare a nutrition assessment, a registered dietitian (or registered dietitian nutritionist), dietetic technician registered, or other trained health-care professional uses:
Historical information
Anthropometric measurements
Physical examinations
Laboratory tests
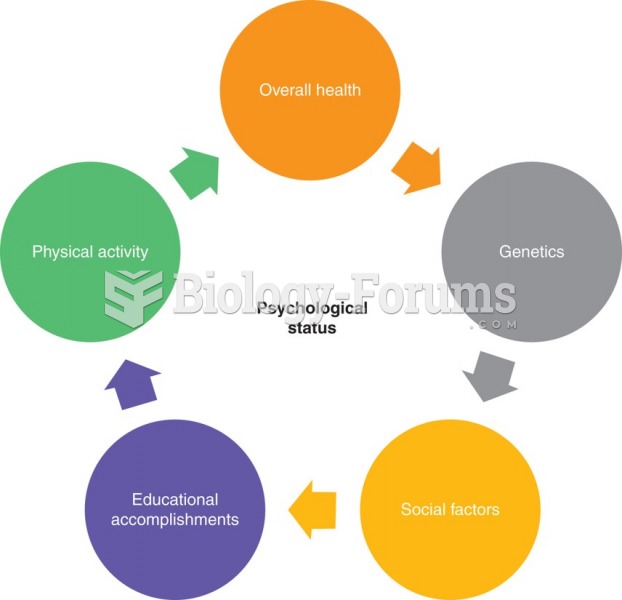
One step in evaluating nutrition status is to obtain information about a person's history with respect to health status, socioeconomic status, drug use, and diet. The health history reflects a person's medical record and may reveal a disease that interferes with the person's ability to eat or the body's use of nutrients. The person's family history of major diseases is also noteworthy, especially for conditions such as heart disease that have a genetic tendency to run in families. Economic circumstances may show a financial inability to buy foods or inadequate kitchen facilities in which to prepare them. Social factors such as marital status, ethnic background, and educational level also influence food choices and nutrition status. A drug history, including all prescribed and over-the-counter medications, may highlight possible interactions that lead to nutrient deficiencies.
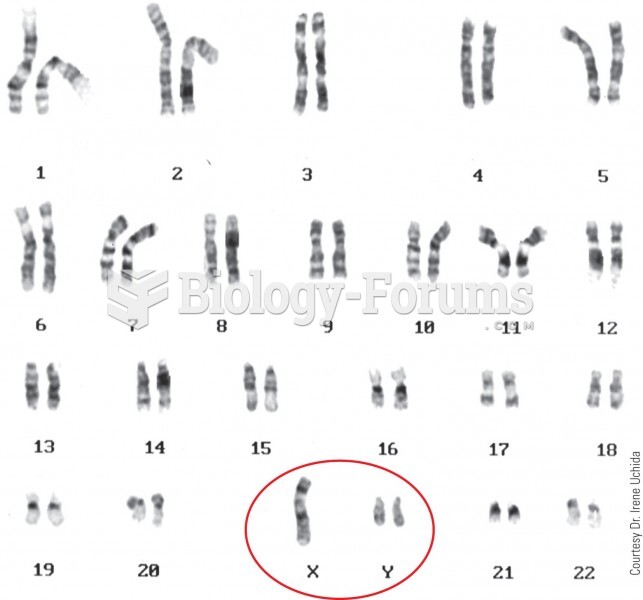
A second technique that may help to reveal nutrition problems is taking anthropometric measures such as height and weight. The assessor compares a person's measurements with standards specific for gender and age or with previous measures on the same individual.
A third nutrition assessment technique is a physical examination looking for clues to poor nutrition status. Visual inspection of the hair, eyes, skin, posture, tongue, and fingernails can provide such clues. In addition, information gathered from an interview can help identify symptoms. The examination requires skill because many physical signs and symptoms reflect more than one nutrient deficiency or toxicityor even nonnutrition conditions. Like the other assessment techniques, a physical examination alone does not yield firm conclusions. Instead, physical examinations reveal possible imbalances that must be confirmed by other assessment techniques, or they confirm results from other assessment measures.
A fourth way to detect a developing deficiency, imbalance, or toxicity is to take samples of blood or urine, analyze them in the laboratory, and compare the results with normal values for a similar population. Laboratory tests are most useful in uncovering early signs of malnutrition before symptoms appear. In addition, they can confirm suspicions raised by other assessment methods.
Answer to Question 2
Estimated Average Requirements (EAR): The committee reviews hundreds of research studies to determine the requirement for a nutrienthow much is needed in the diet. The committee selects a different criterion for each nutrient based on its roles in supporting various activities in the body and in reducing disease risks.
An examination of all the available data reveals that each person's body is unique and has its own set of requirements. Men differ from women, and needs change as people grow from infancy through old age. For this reason, the commit- tee clusters its recommendations for people into groups based on gender and age. Even so, the exact requirements for people of the same gender and age are likely to be different. Using this information, the committee determines an Estimated Average Requirement (EAR) for each nutrientthe average amount that appears sufficient for half of the population.
Recommended Dietary Allowances (RDA): Once a nutrient requirement is established, the committee must decide what intake to recommend for everybodythe Recommended Dietary Allowance (RDA). The EAR is probably closest to everyone's need. If people consumed exactly the average requirement of a given nutrient each day, however, approximately half of the population would develop deficiencies of that nutrient. Recommendations are therefore set greater than the EAR to meet the needs of most healthy people.
Adequate Intakes (AI): For some nutrients, such as vitamin K, there is insufficient scientific evidence to determine an EAR (which is needed to set an RDA). In these cases, the committee establishes an Adequate Intake (AI) instead of an RDA. An AI reflects the average amount of a nutrient that a group of healthy people consumes. Like the RDA, the AI may be used as nutrient goals for individuals.
Tolerable Upper Intake Levels (UL): The recommended intakes for nutrients are generous, yet they may not be sufficient for every individual for every nutrient. Nevertheless, it is probably best not to exceed these recommendations by very much or very often. Individual tolerances for high doses of nutrients vary, and somewhere beyond the recommended intake is a point beyond which a nutrient is likely to become toxic. This point is known as the Tolerable Upper Intake Level (UL).