Answer to Question 1
Goal: Maintain optimal metabolic outcomes to prevent micro- and macrovascular complications.
Glucose levels in normal ranges:
Fasting: 80-110 mg/dL
Preprandial: 80-130 mg/dL
Postprandial: <180 mg> A1c: < 7
Normalize lipid or lipoprotein profile to reduce risk of cardiovascular disease (cholesterol and triglyceride values are high in patient's lab reports)
Optimize blood pressure levels
Modify lifestyle habits including dietary intake and physical activity to prevent further complications.
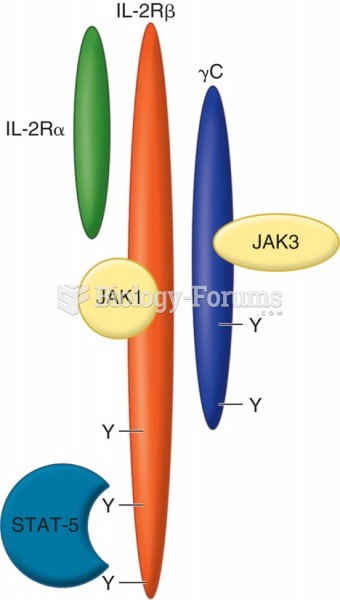
Intensive insulin therapy with TDD 30 units, 15 units basal, and ICR 17g:1 unit rapid-acting insulin
Integrate insulin therapy with Matias's food and physical activity preferences
Respect Matias's wishes, willingness, and ability to change (can eat a generally normal diet)
Educate him on the signs and symptoms of hypoglycemia and how to treat it
Promote the consumption of a general healthy diet
Answer to Question 2
Matias's mother is most likely experiencing retinopathy and neuropathy secondary to T2DM and chronic hyperglycemia.
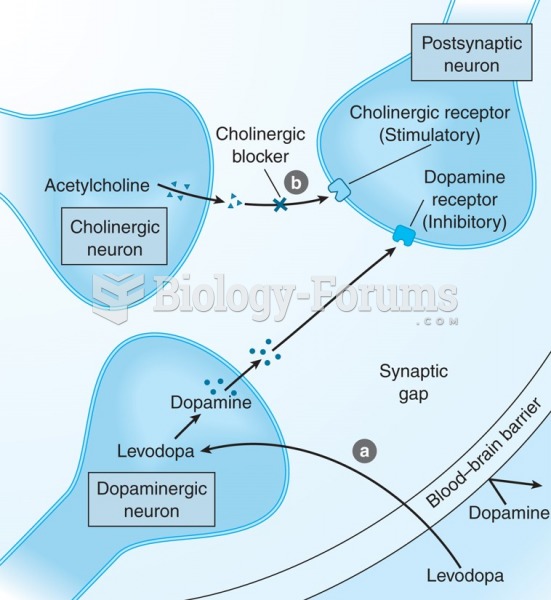
Poorly controlled blood glucose levels can lead to a state of chronic hyperglycemia, which causes further complications such as retinopathy and neuropathy.
Hyperglycemia results in increased production of sorbitol, which cannot cross the cell membrane. The accumulation of sorbitol damages blood vessels of the eye, leading to macular edema, glaucoma, and possible blindness.
In general, hyperglycemia changes the structure of the blood vessels, causing endothelial damage to the vessels, whether the blood vessels are microvascular or macrovascular.
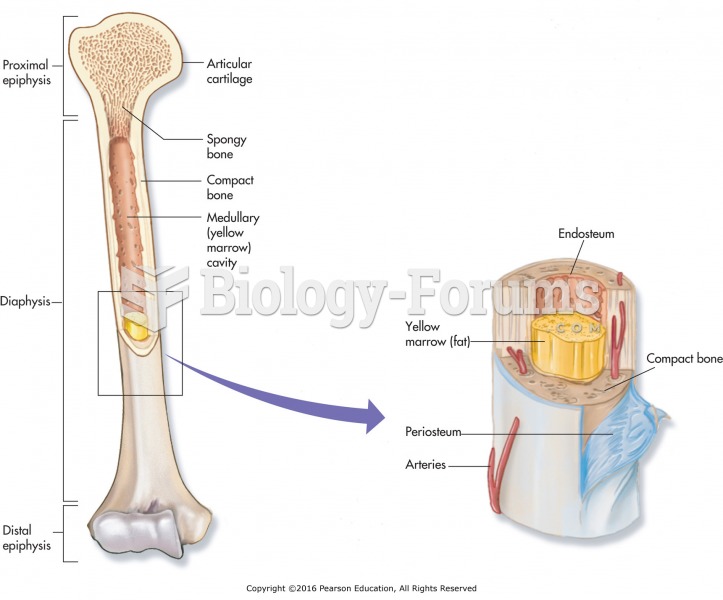
The basement membrane of the blood vessels thickens, affecting the blood flow, especially to the extremities. This increased resistance increases blood pressure and work of the heart.
Hyperglycemia results in abnormal amounts of glycated proteins that damage nerve structure and function.
The DCCT determined that in T1DM patients who improve glycemic control, complications associated with damaged vessels may be delayed or even prevented.
There was a 60 reduction in microvascular neuropathy in those who used intensive insulin therapy for glycemic control compared to conventional therapy, and a 63 reduction in retinopathy. These numbers were significant.
The EDIC study was a follow-up study using the same participants as the DCCT that demonstrated further reductions in the percentage of microvascular complications over a longer period of time.
Using this information from these studies in type 1 diabetics, Matias can prevent complications, especially microvascular complications, by being compliant with intensive insulin therapy. If he can control his blood glucose levels, the risk for complications decreases.