Answer to Question 1
Hypoglycemia is defined as a blood glucose level of less than 70 mg/dL according to the American Diabetes Association. In other words, it is low blood sugar.
Symptoms associated with hypoglycemia include:
Weakness
Shakiness
Perspiration
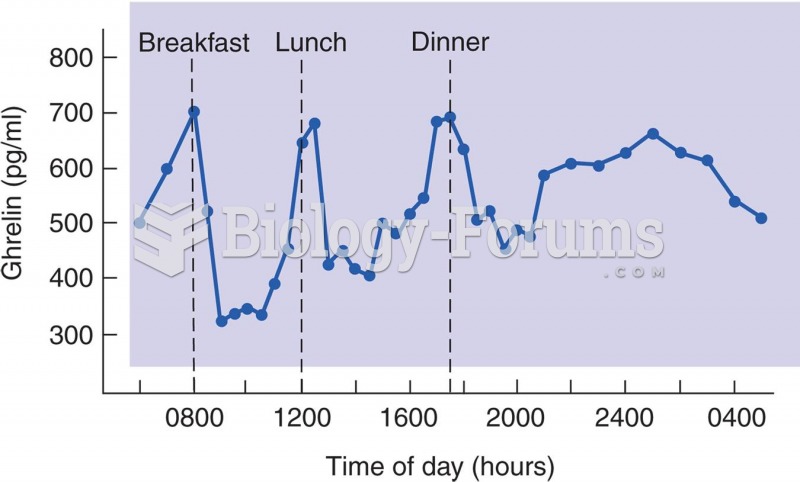
Hunger
Rapid heartbeat
Symptoms are individual and vary from person to person
If severe, altered mental status may occur (may lose consciousness)
Remedy for mild hypoglycemia is the 15/15 rule:
First, Matias should be able to identify signs and symptoms associated with hypoglycemia.
Matias would be instructed to monitor his blood glucose level. If he has a low reading (<70 mg>Matias would consume a food/beverage providing 15 g of rapid-acting carbohydrates such as cup fruit juice, 3-4 glucose tablets, etc.
If blood sugar is below 50 mg/dL, 20-30 g of carbohydrate should be consumed.
Then Matias should wait 15 minutes and re-check his blood glucose. If it is still low, he should consume 15 g more of carbohydrates and the process should be repeated.
If he has exercised, if he will not eat within the next hour, or if he is going to bed, an additional snack may be needed.
Severe hypoglycemia cannot be self-treated with the 15/15 rule. Thus, having him inform his friends and family of the signs of what to look for and how to treat hypoglycemia can be life-saving.
Determine that he feels comfortable with recognizing his personal signs and symptoms of hypoglycemia before it becomes too severe to self-treat.
Determine awareness that exercise can make one prone to hypoglycemia, especially strenuous exercise lasting a longer duration. Ensure that he knows appropriate equipment to keep on hand during exercise: personal and diabetes information, carbohydrate snack.
- Liquid, soft, or otherwise easily chewed/swallowed simple carbohydrate options will allow quick and easy administration (for himself and others if their assistance is needed).
Answer to Question 2
Intensive insulin therapy is a flexible insulin regimen compared to conventional or standard therapy. Conventional is a fixed insulin dose whereas intensive insulin therapy uses SBGM to determine how much insulin to give at meal times plus it uses a basal insulin dose based on the patient's weight.
Intensive insulin therapy requires multiple daily injections of bolus insulin before meals in addition to basal insulin once or twice daily.
Intensive insulin therapy, when compared to standard therapy, has demonstrated better glycemic control but it requires patients to self-monitor their blood glucose levels.
Barriers to success:
Compliance with giving multiple daily injections
Compliance with checking blood glucose levels in the morning, preprandially and post-prandially
Learning to carbohydrate count
Inconvenience of carrying glucometer with normal daily living activities
Learning how to accurately use glucometer and how to calculate insulin dosages needed
Lack of support system
Fear of hypoglycemia
Health practitioners can help the patient overcome barriers by providing education and support
Educate patient on how to effectively use glucometer. Have patient practice on himself and the dietitian to make sure he understands the proper technique to monitor blood glucose.
Educate patient on carb counting. Have patient develop sample meals to demonstrate that patient understands the process of carb counting. Providing the patient with the Exchange List booklet can be beneficial.
Have patient practice injections.
Give patient recording tools such as graphs and charts that may help the patient keep track of physical activity, blood glucose levels, and carbohydrate intake.
Teach patient about signs/symptoms of hypoglycemia and the appropriate treatment.
Help patient develop appropriate target blood glucose ranges using the ADA guidelines.
Refer to SBGM as monitoring and avoid saying the word testing.