Answer to Question 1
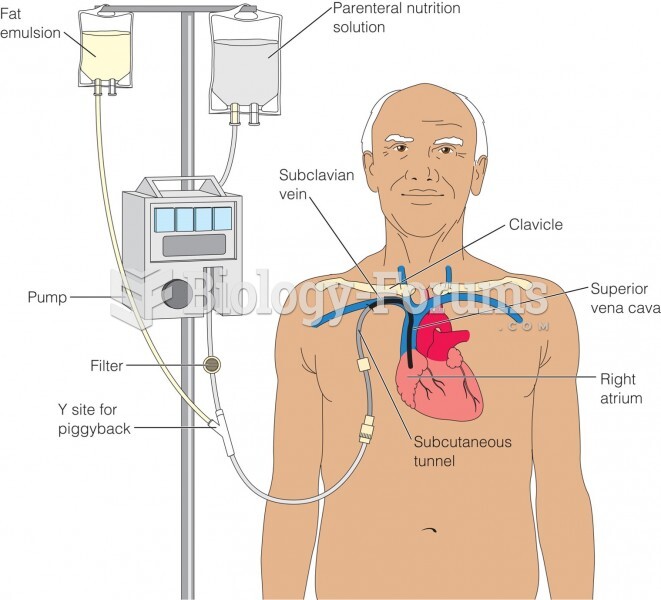
Inadequate oral intake related to acute pancreatitis as evidenced by N/V, abdominal pain, dry skin and mucous membranes, poor skin turgor, patient self-report of limited oral intake 3 days PTA, and NPO status since admission.
Altered GI function related to compromised exocrine function of pancreas as evidenced by recent diagnosis of acute pancreatitis and current NPO status.
Increased nutrient needs related to compromised pancreatic function as evidenced by C-reactive protein of 141 mg/dL and diminished albumin level of 3.3 g/dL consistent with increased stress and metabolic requirements.
Answer to Question 2
Surgery can affect nutritional status in a variety of ways depending on where it is performed.
In the case of gastric cancer, a partial or total gastrectomy increases a patient's risk for vitamin B12 deficiency.
- Calcium and iron absorption will also be reduced.
- Dumping syndrome, delayed gastric emptying, early satiety, nausea, and vomiting may also occur as a result.
Surgery to treat intestinal cancer may cause malabsorption of nutrients and steatorrhea.
In general, patients undergoing surgery may require additional calories and protein for wound healing.
Radiation therapy to the head and neck area can cause the following, all which can all make consuming an adequate diet difficult:
- Mucositis
- Dysgeusia
- Xerostomia
- Dysphagia
- Odynophagia
- Severe esophagitis
Because radiation therapy damages the epithelial cells the body's ability to digest and absorb nutrients may be impaired.
Radiation to the abdominal and pelvic area can cause diarrhea, nausea, and vomiting.
Chemotherapy greatly affects cells with a high turnover rate and thus have effects on the cells of bone marrow, the epithelial lining of the GI tract, and the hair follicles. The most common side effects include:
- Neutropenia, thrombocytopenia, anemia
- Diarrhea
- Mucositis
- Alopecia