Answer to Question 1
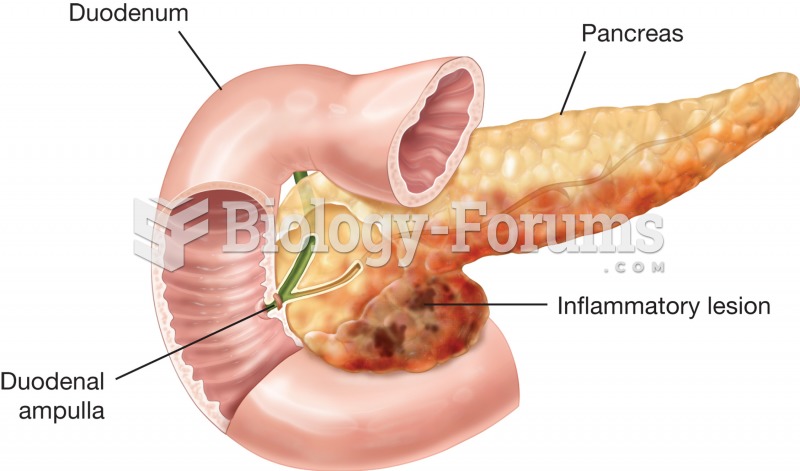
Alcohol plays a significant role in the pathogenesis of pancreatitis. Chronic, heavy alcohol ingestion diminishes the concentration of lithostathine, a secretory protein that helps solubilize calcium carbonate within the pancreatic ducts. As a result, there is a build-up in ductile pressure that damages acinar cells and releases pancreatic enzymes into the periacinar space.
Another theory is that prolonged alcohol intake leads to the fusion of zymogen granules (which contain inactive pancreatic enzymes) with lysozomes that contain hydrolytic enzymes and results in activation of the pancreatic enzymes, leading to autodigestion of the pancreas.
The exact mechanisms that lead to pancreatic injury are not fully understood, but a common characteristic appears to be a premature activation of trypsin within the pancreas, resulting in autodigestion of pancreatic cells. Enzymes released by destroyed pancreatic cells eventually reach the bloodstream, causing elevated serum amylase and lipase levels.
Other conditions associated with acute pancreatitis include hypercalcemia, hypertriglyceridemi a, drugs, trauma, cystic fibrosis, renal failure and other, infectious causes.
Factors in the history and physical that are consistent with acute pancreatitis include: chief complaint; fever; increased pulse and blood pressure; hyperactive bowel sounds x4; extreme tenderness, rebound, and guarding; nausea and vomiting; and history of alcohol use.
Answer to Question 2
Some studies suggest that a plant based diet can be beneficial due to the potential benefits of increased fiber, fruit, and vegetable intake (especially in regards to polyphenol/phyto-estrogen-rich foods).
Additionally, a plant based diet will avoid red meat's suspected increased risk toward increasing cancer risk.
Vitamin D supplementation may be needed if not a lacto-vegetarian