Answer to Question 1
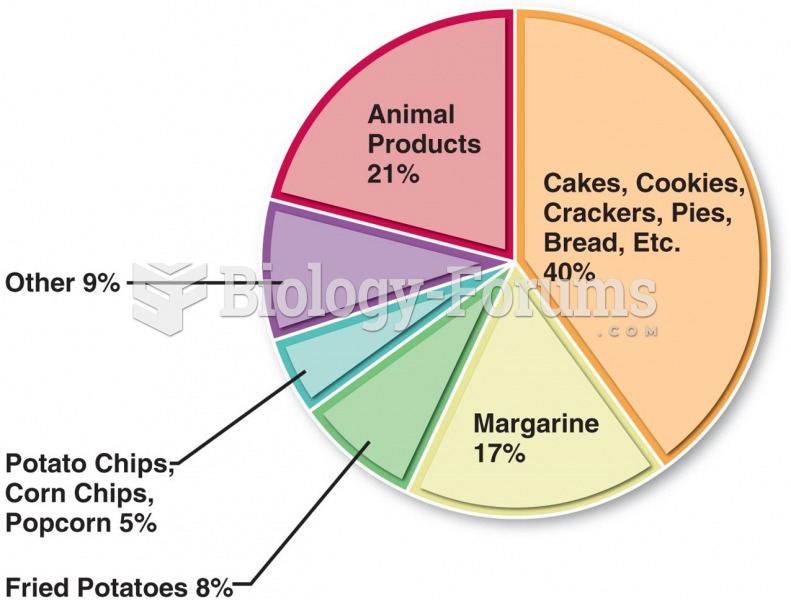
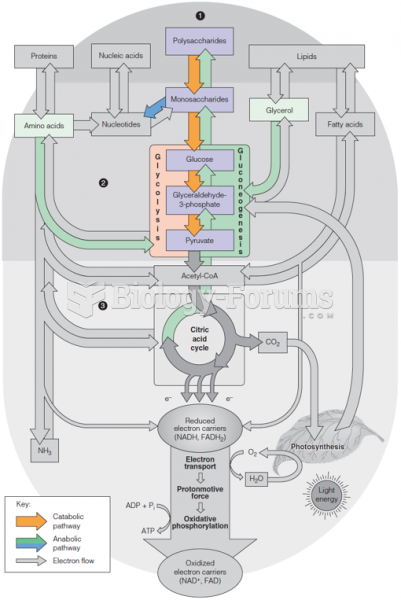
High-carbohydrate diets may lead to hepatic insulin resistance by activating carbohydrate responsive element binding protein (ChREBP), inducing glycolysis and lipogenic pathways within liver tissue
Answer to Question 2
DATE/TIME
A: 37 yo M
Admitted with SOB now on mechanical ventilation with probable sepsis
PMH: T2DM, HTN, Hyperlipidemia, Osteoarthritis
PSH: s/p Roux-en-Y bariatric surgery 4 months previously, total knee replacement
Meds: lovastatin 60 mg/day (d/c Lantus and metformin 2 months ago)
Skin: warm, dry to touch; ecchymosis, abrasions, petechiae on lower extremities, 2+ pitting edema
Abdomen: obese appearance with rashes under skinfolds; soft, active bowel sounds
I/O: +1430 mL
Labs: K 5.8, CO2 31, Glu 385, Phos 2.1, Pro 5.8, Alb 1.9, Prealb 11, Ammonia 35, WBC 23.5, CRP 110, Ferritin 14, Transferrin 385, Lactate 4.2, Fibrinogen 525, Hgb 12.5, Hct 38, TG 245
Urine: Pro +, Glu +, Ket +, Bact +, WBC +
Diet: NPO
Diet Hx: unable to speak to patient due to mechanical ventilation. Hx of childhood obesity. Patient's highest historical weight was 425 lbs recent weight loss of 76 after bariatric surgery.
Ht: 5'10 Wt: 325 UBW: 425 UBW: 76 IBW: 166 IBW: 196 BMI: 46.7 kg/m2
EER: 1660-1886 kcal/d (based on 22-25 kcal/kg IBW); EPR: 151-189 (based on 2.0-2.5 g/kg/IBW)
D: Predicted suboptimal energy intake related to induced sedation as evidenced by an order for nothing by mouth and mechanical ventilation status.
I: Goal to meet 100 nutritional needs via enteral feeding.
When medically able, recommend a post-pyloric feeding tube to prepare for enteral feeding.
Within 24-48 hours after hemodynamically stable, initiate Peptamen Bariatric 20 mL/hour. Increase as tolerated by 10-20 mL every 8-12 hours until goal rate of 80 mL/hour (based on 22 hours per day -ICU protocol). This will provide daily 1760 mL total volume, 1760 total kcalories, 164 g protein, and 1478 mL free water. Provide approximately 5 flushes of 60 mL free sterile water throughout the day (ever 4 hours).
Make HOB elevated between 30-45 degrees.
Communicate with team the nutrition support recommendations per above.
M/E: RD to follow patient in ICU.
Monitor weight changes, I/O, abdominal sounds, and GI tolerance.
Monitor BG and suggest insulin therapy if consistently above 180 mg/dL.
Monitor lab trends and risks for refeeding syndrome.
Reassess enteral feeding needs once weaned off of ventilator.