Answer to Question 1
Refeeding syndrome is a term used to describe metabolic changes that occur as a result of repletion of malnourished individuals. Refeeding syndrome occurs after a period of starvation to which the body has adapted by metabolizing fat for energy instead of carbohydrate. When a carbohydrate-rich diet is reintroduced, thiamin, phosphorous, potassium, and magnesium are swiftly removed from the bloodstream into the cells for anabolism.
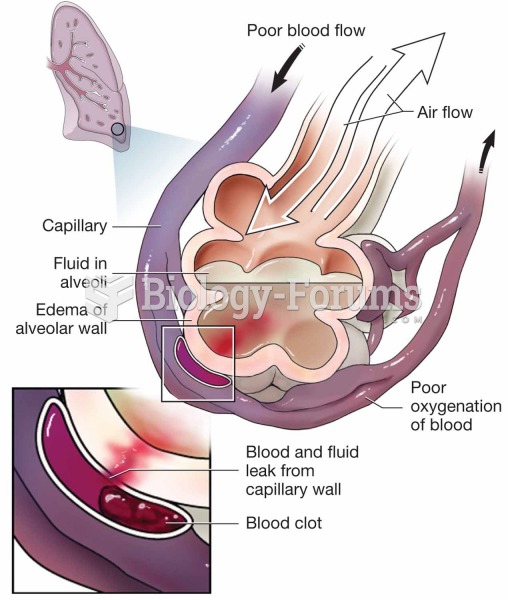
This may result in electrolyte imbalances and shifts of fluid balance that accompany these changes. This can lead to heart failure and edema, acidosis, hyperventilation, and neurological dysfunction.
Mr. Page is at risk due to his malnutrition, metabolic stress, and levels of electrolytes.
Prevention of refeeding can be prevented by following these steps:
1) Obtain and correct baseline electrolytes (supplement K, Phos, Mg).
2) Initiate nutrition support with caution and at a low and slow rate (e.g., 15-20 kcal/kg or 3) Increase caloric intake gradually.
4) Monitor electrolytes closely (q 12 hr; 2x/day) for at least the first 3-5 days until Mr. Page is stable at his full caloric target.
Answer to Question 2
Increased energy expenditure: Patient with extensive tissue and inhalation injury resulting in increased metabolic and catabolic state. Patient cannot meet the nutritional demands due to mechanical ventilation and need for consistent intake that is very high in calories and high biological value protein.
Inadequate enteral nutrition infusion: Even with initiation of continuous enteral nutrition patients will have multiple interruptions due to dressing changes, rehab therapy, surgery, and tests/procedures. Due to the hypercatabolic state and high rate of gluconeogenesis, patients will break down lean body mass to fuel the glucose production. An average adult loses about 60-70 g of protein with simple fasting, which is about 240-280 g of lean body mass. With high-metabolic demand states like the burn injury, patients may lose up to 600-1000 g of muscle mass a day.