Answer to Question 1
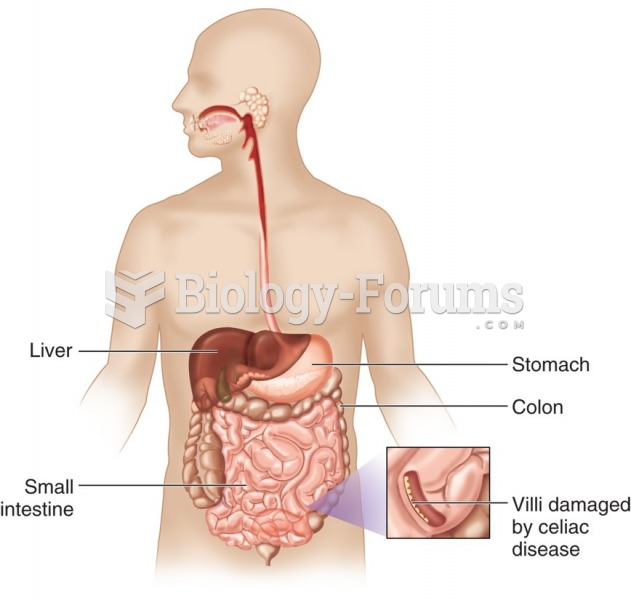
Inflammatory bowel disease (IBD) is a chronic relapsing inflammatory condition involving the gastrointestinal tract; the term IBD encompasses the two specific diagnoses of Crohn's disease and ulcerative colitis (UC). IBD is thought to involve the activation of T cells (by macrophages) to produce a T H1 immune response (cytokine production) that causes a vicious cycle of chronic inflammation. The mucosal damage from the abnormal immune response can allow the translocation of luminal contents past the tight junctions. This can allow the body to produce antigens to these leaked in contents. . The etiology of IBD is still unclear, but it is believed that various environmental factors may be involved as triggers for the inflammatory response of the disease; genetics also play an important role in the etiology of the disease. Certain genes are linked to the dysregulation of the gastrointestinal immune response and microbiome and therefore certain individuals are more susceptible than others to develop IBD. IBD has been found to be more prevalent among individuals of Caucasian and Ashkenazi Jewish descent. However, because all genetically susceptible individuals do not develop IBD, and because of the speed at which IBD incidence has increased in certain regions of the world, genetics cannot be the sole factor in the etiology of IBD. Proposed theories regarding the environmental factors associated with IBD involve the hygiene hypothesis, Helicobacter pylori, family size and birth order, urban environment, etc. Smoking, oral contraceptives, appendectomy, diet, breastfeeding, and nonsteroidal anti-inflammatory drugs (NSAIDs).
Answer to Question 2
Alicia Clarke (Nutrition consult for IBS)
7-10-12
A: 42 YOWF Dx: irritable bowel syndrome-Diarrhea (D); PMH: history of constipation and diarrhea, obesity, GERD, and hypothyroidism
Meds: Omeprazole 50 mg twice daily; Levothroxine 25 mcg; vitamin D 600 IU; 800 mg calcium; Lomotil prn. Elavil (25 mg daily), Metamucil (1 T in 8 oz. of liquid twice daily)
Skin: warm, dry
Abdomen: hyperactive bowel sounds x4; no organomegaly or masses - lower abdominal tenderness.
Labs: glu 115, Chol 201, Tg 171, HDL 42, HbA1C 6.1, Urinalysis: WNL
Height: 5' 5 (65in.), Weight: 191 lbs. BMI: 32 (obese), IBW 125 +/- 10, 153 IBW
Estimated energy requirements: 1250 -1420 kcal (22-25 kcal/kg IBW to facilitate weight loss)
Estimated protein requirements: 46-57 g per day
Diet Hx: diet reveals many fermentable oligosaccharides, disaccharides, monosaccharides, artificial sweeteners, and sugar alcohols are consumed (FODMAP assessment analysis). Snacks are high in fat as evidenced by cookies, cake, and ice cream. Often consumption of gas-producing foods including: asparagus, kidney beans, lentils, fruit juice, dried fruit, artificial sweeteners, and fructose, which may contribute to IBS symptoms. Daily high fiber sources include wheat, dried fruit, kidney beans, and lentils.
D: Nutrition-related knowledge deficit related to FODMAP food consumption as evidenced by FODMAP assessment with frequent consumption of asparagus, sugar alcohols, high-sugar foods, and lentils.
I: Goal: Identify food triggers that make symptoms worse and alleviate symptoms.
pt. will focus on elimination diet and re-introduction over 6-8 week trial.
pt. will be educated on the FODMAP foods to identify which foods may contribute to symptoms.
pt. will consider adding probiotics such as cheese, kefir, or yogurt to diet.
pt. may consider continuing weight reduction to improve overall health.
M/E: pt. will keep a food diary for six weeks to identify food patterns. Pt. should note when symptoms occur to identify food triggers. Pt. should note episodes of diarrhea.
Symptoms will be monitored as pt. eliminates FODMAP foods from diet over a period of time.