Answer to Question 1
Inadequate intake of enteral nutrition as evidenced by nutrition prescription of 25 mL/hour providing only 900 kcal and 56 g protein compared to goal rate of 54 mL/hour providing 1944 kcal and 122 g protein.
- Ideal Goal: Provide enteral nutrition to meet kcal needs of 1900 kcal and 60 g protein.
- Intervention: Modify rate of enteral feeding by increasing goal rate to 54 mL/hour.
Increased nutrient needs related to impaired nutrient utilization of vitamin B12 post gastrectomy (in this case evidence may not be necessary to develop appropriate nutrition care).
- Intervention: Vitamin supplementation; may require order for injection of vitamin.
Evident protein-energy malnutrition related to prolonged inadequate oral/food beverage intake as evidenced by BMI of 20, involuntary weight loss, and pre-albumin of 14 mg/dL.
- Ideal Goal: Weight maintenance and slow, steady weight gain of 1-2 pounds/week and improved pre-albumin to within normal of 18-35 mg/dL.
Food and nutrition-related knowledge deficit related to altered GI function as evidenced by patient requesting nutrition education and concern for special diet forever.
- Ideal Goal: Patient will understand the rationale for advancing oral food from liquid to soft diet as tolerated without adverse symptoms from dumping syndrome.
- Intervention: Nutrition education to include purpose of modification for simple carbohydrates and liquids. Additionally, initially avoiding lactose will be beneficial. Nutrition counseling that provides tools for self-monitoring and social support may also be helpful. (Refer to question 25 below.)
Answer to Question 2
Increased respiratory rate:
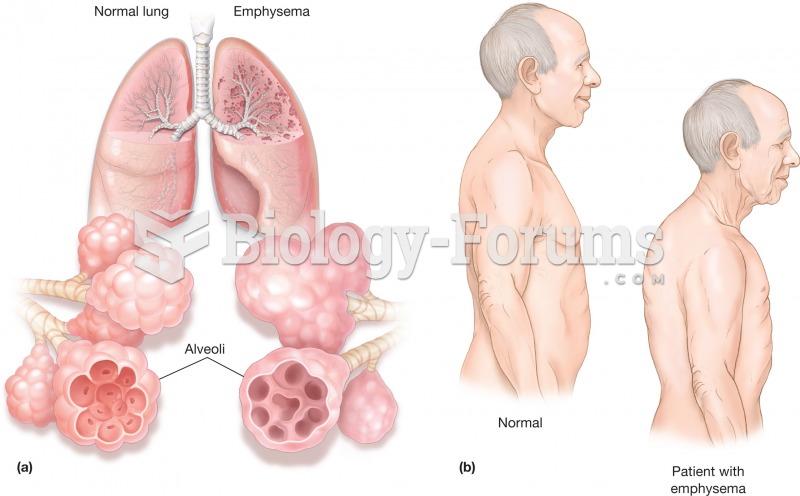
Emphysema damages the elasticity of the airway and destruction of the alveolar wall occurs.
Thus, airways collapse during expiration, which causes air to become trapped.
The lungs and chest wall hyper-expand in an attempt to compensate.
This increases the overall work of breathing and requires more breaths due to this inefficiency.
Jugular distention: Due to the decreased amount of oxygen available, widespread vasoconstriction and increased pulmonary artery pressure occur.
1+ pitting edema of the extremities:
When the heart (R ventricle) has to work harder in response to the decreased overall oxygen saturation, over time the increased pressures are transmitted to the venous circulation.
This results in peripheral edema.
Harsh inspiratory breath sounds: This is due to the trapping of air and the prolonged expiration.
Absent inspiratory breath sounds/hyperresonance of the left chest: This is due to the collapsed lung caused by the tension pneumothorax.
Use of accessory muscles: It is typical for a patient with emphysema to develop use of the accessory muscles (and form a barrel chest) in order to assist with the expiration of air.