Answer to Question 1
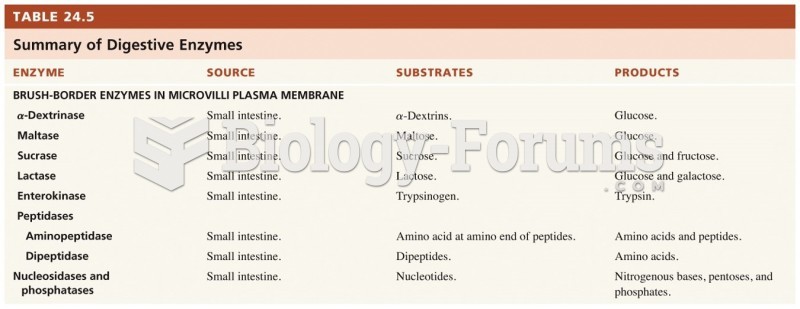
The procedure may change the digestive process both physically and chemically.
The stomach has been partially resected, which will reduce the holding capacity of the stomach.
Gastric emptying may also change depending on the status of the pylorus and the vagus nerve and any other anatomical changes.
Loss of the duodenum reduces the overall surface area for digestion and absorption.
Nutrition concerns include the potential for vitamin and mineral deficiencies.
Possible reductions in gastric acidity may result in inadequate iron absorption (due to the acidic environment being necessary to maintain the reduced ferrous state of iron)
Changes in gastric anatomy may cause inadequate intrinsic factor to be secreted.
- This would prevent normal B12 absorption and lead to a subsequent deficiency.
- Research has confirmed that patients who have had gastric surgery have a high prevalence of vitamin B12 deficiency.
The duodenum is no longer functional but the jejunum will accommodate the functions of the duodenum over time.
Initially there may be a reduction in some enzyme functionspecificall y for lactase (causing typically transient lactose-intolerance).
Finally, transit time is affected, which may result in dumping syndrome.
Answer to Question 2
Shortness of breath (dyspnea)
Emphysema results from irreversible destruction of lung tissue that causes a loss of elasticity in the alveoli.
Healthy alveoli provide a rigid structure to bronchioles that normally allow the airways to remain open.
With emphysema, alveolus tissue loses its elasticity and collapses when air is exhaled.
As alveoli are destroyed, the lungs are able to transfer less and less oxygen to the bloodstream.
Therefore, shortness of breath results.
Early morning confusion (hypercapnia)
If the patient is retaining CO2 (hypercapnia), it is common to see the effects of carbon dioxide toxicity in the a.m.
Overnight, respiratory rate decreases. Therefore, less CO2 is released.
With the pathology of the disease, the patient with emphysema experiences CO2 retention due to the collapse of bronchioles that affects not only inspiration of oxygen but also expiration of CO2
CO2 retention may also increase with loss of muscle mass that allows for support of expiration.
Increased production of brownish-green sputum
Sputum production is common with COPD.
When a patient experiences an increase in production and/or a change in the type of sputum (i.e., color), it is generally one of the first signs of either an exacerbation of the condition (due to chronic bronchitis) and/or an underlying infection.
Fatigue
Fatigue in respiratory muscles occurs because length-tension relationships within respiratory muscles are less than optimal, promoting respiratory muscle inefficiency and fatigue.
Adequate oxygen supports all activity. Without adequate perfusion, the patient experiences fatigue.
As dyspnea worsens, so does fatigue.
Malnutrition contributes to fatigue.
Early satiety
Early satiety occurs when the patient reaches a full or satiated state after only a small ingestion of food.
Patients with COPD most probably experience this symptom due to dyspnea.
Eating also increases pressure on the diaphragm, which contributes to increased dyspnea and consequently early satiety.
Aerophagia (swallowing of air) with gastric retention may also contribute.
Anorexia
Loss of appetite is common in patients with COPD.
Fatigue, dyspnea, and side-effects of medication all may contribute.
Dysgeusia
Taste changes or altered taste may be a result of medications or changes in saliva.
Acid-base imbalances or ketosis may also contribute.
Cigarette smoking may also result in dysgeusia.
Increased blood pressure
Multifactorial
As oxygen saturation drops, the message to the CNS is that circulating blood volume is decreasing.
The sympathetic nervous system is stimulated, resulting in release of norepinephrine.
This causes generalized arterial and venous vasoconstriction and an increase in blood pressure.
Increased respiratory rate
Emphysema damages the elasticity of airway and there is destruction of the alveolar wall.
Thus, airways collapse during expiration, which causes air to become trapped.
The lungs and chest wall hyperexpand, attempting to compensate.
This increases the overall work of breathing.
Jugular distention: Due to the decreased amount of oxygen available, there is widespread vasoconstriction and increased pulmonary artery pressure.
Pedal edema
When the heart (R ventricle) has to work harder in response to the decreased overall oxygen saturation, the increased pressures are transmitted to the venous circulation over time.
This results in peripheral edema.
Decreased breath sounds: This is due to the trapping of air and the prolonged expiration.
Prolonged expiration
Emphysema damages the elasticity of the airway and partially destroys the alveolar wall.
Thus, airways collapse during expiration, which causes air to become trapped.
The lungs and chest wall hyperexpand, attempting to compensate.
This increases the overall work of breathing.
Rhonchi
Rhonchi are added sounds that occur during either inspiration or expiration.
They are caused by air passing through bronchi that are narrowed.
This narrowing could be a result of inflammation or the presence of mucus from the infectious process of her pneumonia.
Wheezing
Occurs due to narrowed airways.
When this occurs, a high-pitched whistling sound is produced.
Use of accessory muscles: It is typical for a patient with emphysema to develop use of the accessory muscles in order to assist with the expiration of air.