Code the following cases for inpatient facility purposes using ICD-9-CM and ICD-10-CM and PCS codes.
Calculate the MS-DRG.
Identify the principal vs. secondary diagnoses and procedures.
Use external cause codes when appropriate.
Do NOT code procedures that are captured by the facility chargemaster.
Secondary diagnoses and procedures do not need to be sequenced in any particular order.
Enter "None" when no code is required.
INPATIENT HOSPITAL
Health Record Face Sheet
Record Number: 78-50-77
Age: 59
Gender: Male
Length of Stay: 4 Days
Service Type: Inpatient
Discharge Status: To Home
Diagnosis/Procedure: Cholelithiasis
Cholecystitis
Total Cholecystectomy
DISCHARGE SUMMARY
PATIENT: PETER INPATIENT
RECORD NUMBER: 78-50-77
ADMITTED: 11-15-XX
DISCHARGED: 11-19-XX
PHYSICIAN: DR. ALEX, M.D.
DISCHARGE DIAGNOSIS: Cholelithiasis.
Acute and chronic cholecystitis.
Gallbladder adhesions.
Allergic reaction to anesthesia.
PROCEDURE: Total cholecystectomy/
Failed attempt laparoscopic cholecystectomy. REASON FOR ADMISSION: The patient is a 59-year-old Caucasian male who was admitted for cholecystectomy for cholelithiasis and cholecystitis. The patient had no admitting lab or x-ray; it had all been done as an outpatient and was all normal.
HOSPITAL COURSE: The patient was taken to surgery where an attempt was made at laparoscopic cholecystectomy. This could not be accomplished because of severe adhesions and an inability to distinguish anatomy in the area. The patient, therefore, underwent an open cholecystectomy. His postoperative course was complicated by an allergic reaction to the anesthesia. The patient had shortness of breath and urticaria all over his body. The patient was treated immediately for the allergic reaction and responded well. By the next morning, the urticaria and shortness of breath had resolved. He is being discharged to be seen in follow up in my office in one week
DISCHARGE INSTRUCTIONS: Discharge diet is regular. He may participate in activity as tolerated except for heavy lifting or straining. The patient is sent home with same medications as previously taken. He may bath or shower and pat his incision dry. The patient is to report any nausea, vomiting, diarrhea, fever, or chills, redness or swelling of his incision. He is not to drive if he takes pain pills. The patient is being discharged in the care of his wife who is capable of taking care of him.
DR. ALEX, M.D.
Electronically authenticated by Dr. Alex, M.D. 11-21-xx 467
HISTORY AND PHYSICAL
PATIENT: PETER INPATIENT
RECORD NUMBER: 78-50-77
ADMITTED: 11-15-XX
DISCHARGED: 11-19-XX
PHYSICIAN: DR. ALEX, M.D.
CHIEF COMPLAINT: Abdominal pain.
HISTORY OF PRESENT ILLNESS: The patient is a 59-year-old Caucasian male who has had known gallbladder disease for the last 8 years with multiple episodes of severe right upper quadrant pain with penetration through to the back accompanied by diarrhea and belching. He has also had intolerance of fatty foods. Symptoms have been getting progressively worse and he is now being admitted for a cholecystectomy.
PAST MEDICAL HISTORY: Usual childhood diseases. Medical diseases: He had an MI approximately 14 years ago. No other medical diseases. Previous surgery was an appendectomy and a coronary artery bypass. He has had multiple small bone fractures. He denies any allergies. He has had no transfusions.
DRUG ALLERGIES: None known.
MEDICATIONS: He takes Lopressor, Pepcid and aspirin.
FAMILY HISTORY: Mother is alive with diabetes and three MI's. His father died of pulmonary embolism. No other history of familial diseases.
SOCIAL HISTORY: The patient is disabled because of back problems. He is married. Does not drink or smoke.
REVIEW OF SYSTEMS: Negative and noncontributory.
PHYSICAL EXAMINATION
VITAL SIGNS:
GENERAL: Demonstrates a well-nourished, well-developed 59-year-old Caucasian male.
HEENT: Normal.
NECK: Supple. Trachea midline. Thyroid is normal. There are no nodes, masses or bruits in the neck. The supraclavicular and infraclavicular regions are clear.
LUNGS: Clear to auscultation and percussion.
CARDIOVASCULAR: Heart regular rhythm without murmur. S1, S2 are normal. No S3, S4.
ABDOMEN: Soft. Bowel sounds are normal. No megaly, masses, hernias, bruits.
SPINE: Straight. No CVA tenderness.
RECTAL: Demonstrates a normal sphincter and no masses.
EXTREMITIES, NEUROLOGICAL /VASCULAR EXAMINATIONS: Normal.
IMPRESSION: Cholelithiasis and cholecystitis.
RECOMMENDATIONS: Laparoscopic cholecystectomy.
DR. ALEX, M.D.
Electronically authenticated by Dr. Alex, M.D. 11-21-xx 467
OPERATIVE REPORT
PATIENT: PETER INPATIENT
RECORD NUMBER: 78-50-77
DATE OF PROCEDURE: 11-15-XX
SURGEON: DR. ALEX, M.D.
PREOPERATIVE DIAGNOSIS: Cholelithiasis with acute and chronic cholecystitis.
POSTOPERATIVE DIAGNOSIS: Cholelithiasis and acute and chronic cholecystitis.
OPERATIVE PROCEDURE: 1. Cholecystectomy with intra-operative cholangiography.
2. Lysis of adhesions.
3. Failed laparoscopic cholecystectomy.
ANESTHESIA: General.
DESCRIPTION: After adequate sedation, the patient was brought to the operating room and placed in the supine position on the operating table. Anesthesia was induced with intravenous Pentothal, endotracheal tube was passed and the patient was maintained on endotracheal anesthesia.
After obtaining proper anesthesia, the patient was prepped and draped in the usual fashion. An infraumbilical incision was made, the Verres needle introduced, and satisfactory pneuma-peritoneum obtained. The 10 mm trochar was then placed through the infraumbilical incision and the camera introduced after which a second 10 mm and two 5 mm ports were placed.
Laparoscopy was performed in the usual fashion and except for a large amount of adhesions to the gallbladder, no pathology was identified. Using sharp and blunt dissection an attempt was made to free the adhesions from the gallbladder. The patient's colon was stuck in this area and in spite of an extensive attempt; it was felt unsafe to proceed any further trying to separate the colon from the gallbladder. It was therefore elected to do the procedure open.
A standard subhepatic incision was accomplished, carried down through subcutaneous tissue. The anterior rectus fascia was divided with a knife, the rectus muscle with a Bovie. The posterior sheath and peritoneum were divided with a knife and the peritoneal cavity entered.
Exploration of the peritoneal cavity was normal. The adhesions to the gallbladder were all carefully taken down after which cystic duct was identified. A clip was placed on its junction with the gallbladder and operative cholangiography performed in the usual fashion and read by the radiologist and myself as being normal. The gallbladder was then taken down in retrograde fashion. Hemostasis was obtained with a Bovie. The cystic artery was clipped twice proximally and once distally and then divided. The gallbladder was then excised.
A 10 mm Jackson-Pratt drain was placed. The wound was irrigated with antibiotic solution. Hemostasis was checked and found to be satisfactory, after which the posterior sheath and peritoneum were approximated with continuous #1 Vicryl. The anterior sheath was approximated with continuous #1 Vicryl. The wound was irrigated with antibiotics, injected with Marcaine after which the skin was approximated with staples.
Sterile dressings were applied.
The patient experienced an allergic reaction to the anesthesia while in the recovery room. Approximately 5 minutes after arriving in recovery, the patient began to experience shortness of breath and allergic urticaria presented all over his body. This allergic reaction was immediately treated with immediate resolution of the respiratory issue. The urticaria had resolved by 9:00 a.m. the following morning.
PATHOLOGY returned with diagnosis of cholelithiasis with acute and chronic cholecystitis.
DR. ALEX, M.D.
Electronically authenticated by Dr. Alex, M.D. 11-21-xx 467
ICD-9-CM diagnosis code(s): PDx_____________________
SDx _____________________
ICD-9-CM procedure code(s): PPx_____________________
SPx_____________________
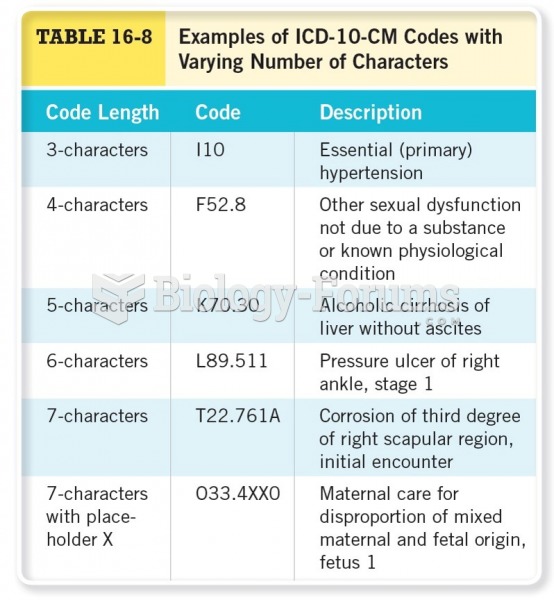
ICD-10-CM diagnosis code(s): PDx_____________________
SDx _____________________
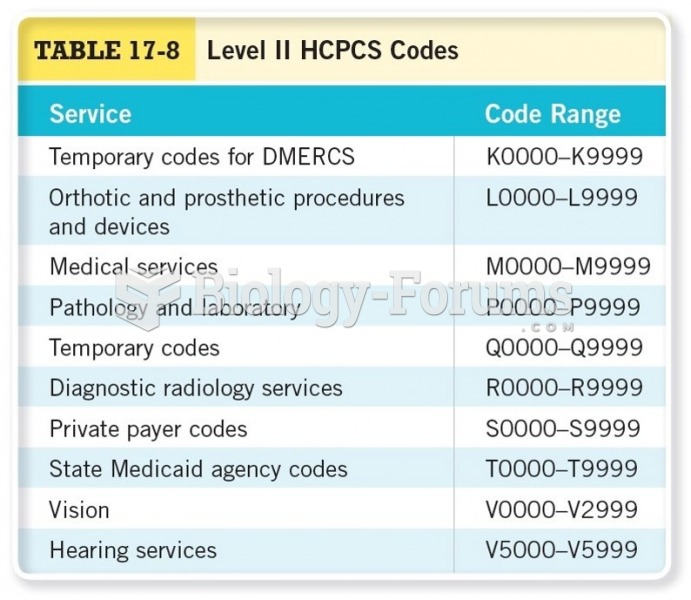
ICD-10-PCS procedure code(s): PPx_____________________
SPx_____________________
MS-DRG: _____________________